The physiology of labour and birth is a complex mechanism involving mother and baby. The relationship between the maternal pelvis and the fetus' head, which is the largest part of the newborn (Marshall and Raynor, 2014), is of great importance for birth without dystocia, a ‘difficult or obstructed labour’ (Neilson et al, 2003). The fetal skull, which completes its ossification process only in early adulthood, is able to adapt to the maternal pelvis through a partial overlapping of the skull bones (a process called moulding), allowing passage during labour without complications (Marshall and Raynor, 2014). Areas such as the occiput and vertex region are used by healthcare professionals to ascertain the fetal position in the maternal pelvis. The diameters of the fetal skull are of great importance for this process, and some are more likely to lead to a birth with favourable outcomes.
Fetal presentation refers to the part of the fetus presenting to the maternal pelvis (Caughey et al, 2015). In a cephalic presentation, vertex presentation being the most common (Makajeva and Ashraf, 2021), the fetal position refers to the position of the occiput in relation to the pelvis (Marshall and Raynor, 2014). In a vertex presentation, the fetal occiput should point towards the maternal symphysis pubis. A persistent occiput posterior fetal position occurs when the fetus' occiput remains in the posterior quadrants of the maternal pelvis during labour and until birth (Barth, 2015).
It is not uncommon for a fetus to begin labour in a posterior position and to rotate to an anterior position before birth: 80–90% of fetuses will spontaneously rotate during labour (Barth, 2015; Masturzo et al, 2017). However, 5–12% will not rotate before birth, leading to a persistent occiput position (Barth, 2015). Occiput posterior is classically diagnosed through an internal digital vaginal examination of the scalp fontanelles. However, studies have shown that this procedure is highly inaccurate (rate of error in second stage of labour: 30–80%), and ultrasonography is more reliable (Simkin, 2010; Barth, 2015).
Occiput posterior is the most common malposition in labour, with reported risk factors including maternal age, race, high body mass index, macrosomia, anterior placenta location, shape of the pelvis and epidural analgesia (Barth, 2015). There is little clarity on the optimal management of occiput posterior position and no agreement among clinicians on the most effective intervention. Specific maternal positions before and after labour are not statistically significantly related to occiput posterior management and resolution (Hunter et al, 2007). The efficacy of manual rotation remains uncertain, despite the safety of the procedure (Phipps et al, 2014; Guerby et al, 2018). Instrumental rotation with Thierry's spatulas appears effective and is associated with low perinatal morbidity, but only if performed by experienced physicians (Phipps et al, 2014). Vacuum extraction has been associated with increased failure compared to rotational forceps, but the latter should only be used by experienced obstetricians (Kahrs et al, 2018).
If repositioning is not possible, then a caesarean section may be carried out; however, this major intervention is related to increased morbidity, especially when performed at full cervical dilatation (Kahrs et al, 2018). The rate of caesarean sections has increased, with attempts to reduce this rate proving largely unsuccessful (Shaffer et al, 2006). According to the World Health Organization (WHO, 2018), this trend has not been accompanied by significant perinatal benefits and may be associated with short- and long-term perinatal risks. Furthermore, caesarean section is associated with higher healthcare costs (WHO, 2018). The controversy of operative births is amplified by the occurrence of severe perineal lacerations, which have been associated with feelings of guilt, anxiety and a sense of loss, which may lead to depression and poor self-esteem among women (Priddis et al, 2014).
The association between occiput posterior position and adverse outcomes is ambiguous, with uncertainty around the best management of this fetal malposition in labour, and no real effective actions are promoted by regulatory institutions. Manual rotation is a safe and cost-effective procedure, but little is known about this manoeuvre and it is practised by few medical professionals (Allahbakhshi Nasab et al, 2023). In order to promote further knowledge and practice on manual rotation, more evidence on the risks associated with persistent occiput posterior needs to be prioritised. The aim of this systematic review was to identify if, in singleton term pregnancies, a persistent occiput posterior fetal position at birth was associated with increased adverse maternal and neonatal outcomes, when compared to births in occiput anterior position.
Methods
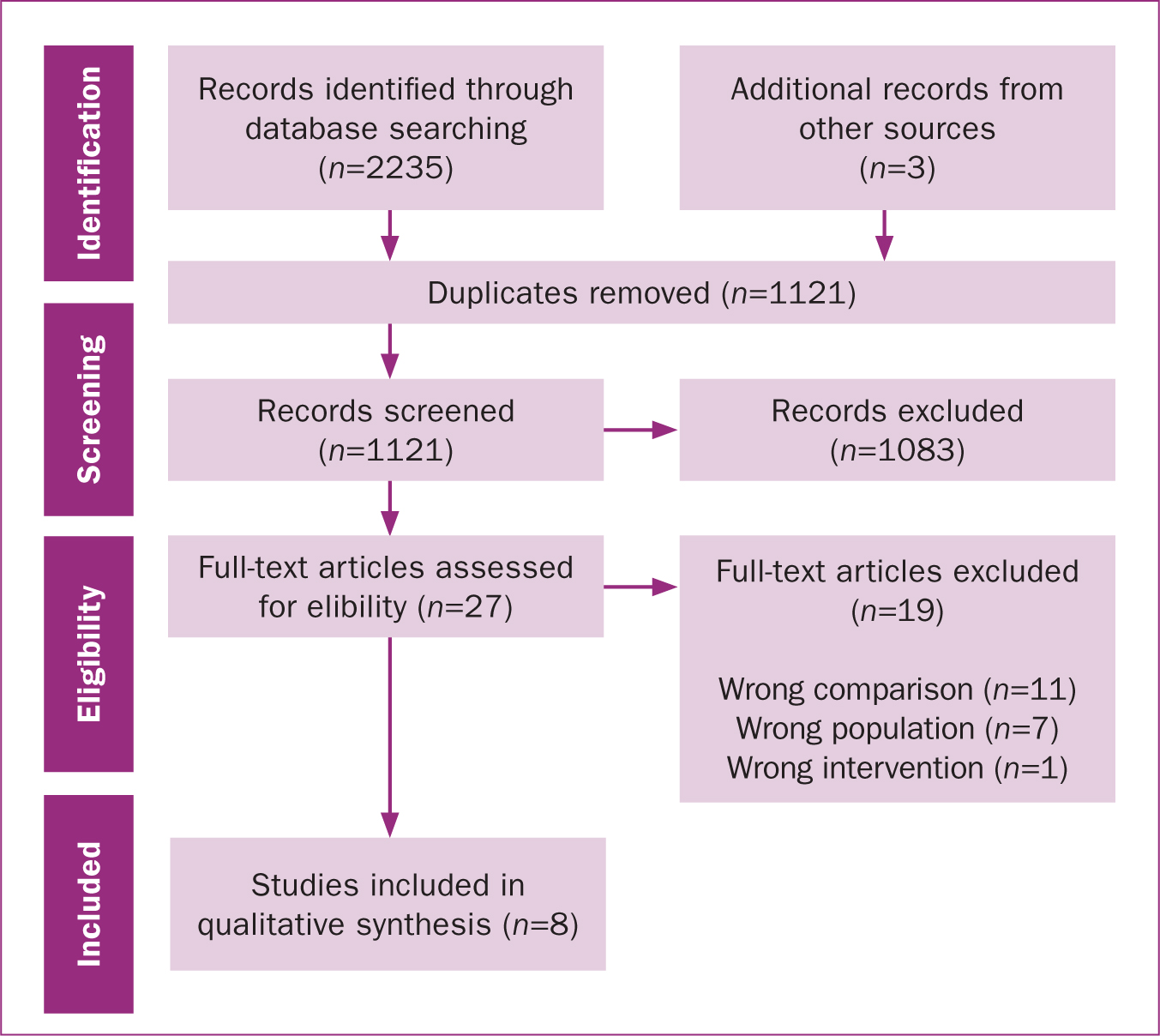
Meta-analysis is a quantitative, formal, epidemiological study design used to systematically assess the results of previous research to derive conclusions about that body of research (Haidich, 2010). This systematic review was produced according to the Cochrane handbook standards (Higgins et al, 2009). The PRISMA checklist was used for reporting (Moher et al, 2009) (Figure 1).
Exposure and outcomes
The exposure was persistent occiput posterior fetal position, defined as the presenting fetal part identified by a clinician at full cervical dilatation by manual vaginal examination or ultrasound abdominal examination, and compared with occiput anterior position. The most commonly reported outcomes in the literature were chosen from Devane et al's (2007) list, and included caesarean section, maternal death (WHO, 2023a), neonatal death (WHO, 2023b), postpartum blood loss (WHO, 2012), third and fourth degree perineal tear (Royal College of Obstetrician and Gynaecologists, 2015), length of labour in hours, chorioamnionitis (Tita and Andrews, 2010), postpartum infection (WHO, 2015), Apgar score at 5 minutes (American Congress of Obstetricians and Gynecologists (ACOG), 2015), umbilical cord gas pH (Yeh et al, 2012), metabolic acidaemia, (ACOG, 2006), admission to neonatal intensive care unit, birth trauma (Ojumah et al, 2017), spontaneous vaginal birth, instrumental birth, oxytocin augmentation (WHO, 2014) and neonatal morbidity, which was subsequently included as a composite variable including Apgar score <7 at 5 minutes, pH <7.00, metabolic acidaemia and admission to neonatal intensive care unit.
Literature search
Prospective and retrospective cohort studies were included, with no publication, language, or date restrictions. The inclusion criteria selected for studies that examined the association between persistent occiput posterior and occiput anterior position, and reported perinatal outcomes in singleton pregnancies between 37 and 42 weeks' gestation. Both nulliparas and multiparas were included. Pregnancy complications were not excluded, unless contraindicating a vaginal birth.
The online databases searched were MEDLINE, EMBASE, Scopus, CINHAL Plus, Global Health and Cochrane Library. The search and eligibility assessment were un-blinded. An adapted ROBINS-I tool (risk of bias in non-randomised studies - of interventions) (Sterne et al, 2016) was used to assess the risk of bias for each study.
Search results
The initial literature search identified 2238 studies (Figure 1). After removal of duplicates, 1121 studies were screened for title and abstract, and 1083 studies were excluded. A total of 27 studies were full-text reviewed and assessed for eligibility; 19 studies were excluded at this stage as they did not make the comparison under investigation (n=11), did not have the selected population (n=7) or did not include the selected intervention (n=1).
Eight studies were included in the final analysis (Table 1), which were conducted between 2000 and 2017 in the UK, Ireland, USA, Canada, Australia, Sweden and Israel. Of these cohort studies, two were prospective and six were retrospective. The range of outcomes examined varied across studies, with older studies more commonly focusing on maternal outcomes, and more recent ones focusing on neonatal outcomes. Confounding in the analysis was addressed only in more recent studies.
Table 1. Characteristics of included studies
| Study | Design | Population | Exposure | Outcome |
|---|---|---|---|---|
| Sizer and Nirmal, 2000 | Retrospective | 16 781 nulliparas (UK) | Birth face-to pubes, or labour requiring rotation from occiput posterior | Apgar scoreMode of birthOxytocin augmentation |
| Fitzpatrick et al, 2001 | Prospective | 13 789 nulliparas and multiparas (Ireland) | Persistent occiput posterior at birth | Perineal lacerationProlonged labourMode of birthOxytocin augmentation |
| Ponkey et al, 2003 | Retrospective | 6434 nulliparas and multiparas (USA) | Occiput posterior recorded at the start of the birth | Perineal lacerationProlonged labourMode of birthOxytocin augmentation |
| Senécal et al, 2005 | Randomised controlled trial, nested retrospective | 1608 nulliparas (Canada) | Occiput posterior at full dilatation at the time of randomisation | Postpartum excessive blood lossPerineal lacerationLength of labourPostpartum feverApgar scoreArterial cord pHNeonatal intensive care unit admissionNeonatal traumaMode of birthOxytocin augmentation |
| Cheng et al, 2006a, b | Retrospective | 31 392 nulliparas and multiparas combined (USA) | Occiput posterior at birth | Postpartum excessive blood lossPerineal lacerationProlonged labourChorioamnionitisApgar scoreArterial cord pHArterial cord base excessUmbilical gas acidaemiaNeonatal intensive care unit admissionNeonatal traumaNeonatal morbidityMode of birthOxytocin augmentation |
| Carseldine et al, 2013 | Double-blinded prospective | 160 nulliparas and multiparas combined (Australia) | Occiput posterior through transabdominal ultrasound within 30 minutes of first vaginal examination at full dilatation | Postpartum excessive blood lossPerineal lacerationLength of labourApgar scoreArterial cord pHNeonatal intensive care unit admissionMode of birth |
| Dahlqvist and Jonsson, 2017 | Retrospective | 27 648 nulliparas and multiparas combined (Sweden) | Occiput posterior at birth | Apgar scoreArterial cord pHNeonatal intensive care unit admissionNeonatal traumaNeonatal morbidityMode of birthOxytocin augmentation |
| Yagel et al, 2018 | Retrospective | 42 778 nulliparas and multiparas combined (Israel) | Occiput posterior at birth recorded in the emergency room | Postpartum excessive blood lossLength of labourApgar scoreArterial cord pHNeonatal intensive care unit admissionMode of birth |
Quality of the evidence
The quality of evidence was assessed through the GRADE evidence profiles (Guyatt et al, 2011), and studies were reviewed according to the STROBE statement (von Elm et al, 2007). Full data for these assessments are available from the authors on reasonable request. All included studies were able to report most required items as per guidelines, but earlier studies failed to report significant items in the methods and discussion sections, such as efforts to reduce bias, sample size calculations, limitations and generalisability of the study. Half of the studies had a severe overall risk of bias, with the remaining half having moderate risk. The severe risk was largely the result of the lack of adjustment for confounding. Missing data were minimal in most studies. Only one study used ultrasonography to assess fetal position in labour. No data on maternal or neonatal deaths were recorded in any of the studies.
Data analysis
An inverse variance, random-effect meta-analysis was performed for each outcome, and a forest-plot reported. Subgroup analyses by parity were performed where available; this particular subgroup analysis was conducted as multiparity is associated with lower risk of adverse birth outcomes (Lin et al, 2021). Analyses were performed on unadjusted data, and on adjusted data where available. Results were reported as odds ratios for dichotomous data, and mean differences for continuous data, with 95% confidence interval and a two-sided P value of 0.05.
Results
Table 1 includes data on the outcomes reported in each study and the population (primiparous, multiparous, combined) included. Full data on the calculated odds ratios based on each individual study's results are available from the author on reasonable request. Heterogeneity was significantly high for most of the outcomes, but when results adjusted for covariates were available, the heterogeneity decreased. Table 2 outlines the effect sizes for all outcomes based on the eight included studies. Almost all outcomes were significantly associated with position, in either or all of primiparous, multiparous or mixed groups of women.
Table 2. Outcome effect size
| Outcome | Parity | Effect size (confidence interval) | P value |
|---|---|---|---|
| Caesarean section* | Primiparas | 4.98 (3.74–6.65) | <0.001 |
| Multiparas | 6.85 (3.81–12.30) | <0.001 | |
| Combined | 6.74 (2.64–17.23) | <0.001 | |
| Postpartum blood loss (ml)† | Primiparas | 0.28 (0.09–0.46) | 0.004 |
| Multiparas | 0.15 (-0.16–0.46) | 0.340 | |
| Combined | 0.28 (-0.03–0.58) | 0.070 | |
| Third and fourth degree perineal tear* | Primiparas | 2.57 (1.34–4.94) | 0.005 |
| Multiparas | 6.61 (0.63–68.95) | 0.110 | |
| Combined | 3.08 (1.67–5.69) | <0.001 | |
| Length of total labour (hours)† | Primiparas | 0.71 (0.34–1.08) | <0.001 |
| Multiparas | 1.97 (-1.26–5.20) | 0.230 | |
| Combined | 0.85 (0.28–1.42) | 0.004 | |
| Length of first stage labour (hours)† | Primiparas | 0.28 (-0.04–0.59) | 0.080 |
| Multiparas | 0.22 (0.00–0.44) | 0.050 | |
| Combined | 0.48 (0.42–0.54) | <0.001 | |
| Length of second stage labour (hours)† | Primiparas | 0.74 (0.59–0.89) | <0.001 |
| Multiparas | 1.27 (1.06–1.48) | <0.001 | |
| Combined | 0.55 (0.29–0.81) | <0.001 | |
| Adjusted | 0.46 (0.40–0.52) | <0.001 | |
| Chorioamnionitis* | Combined | 3.77 (3.36–4.23) | <0.001 |
| Feverish infection* | Combined | 2.53 (1.26–5.10) | 0.009 |
| Apgar score at 5 minutes† | Unadjusted | 0.35 (0.23–0.47) | <0.001 |
| Adjusted | 0.24 (0.12–0.36) | <0.001 | |
| Arterial umbilical cord pH† | Unadjusted | 0.45 (0.23–0.68) | <0.001 |
| Adjusted | 0.30 (-0.12–0.73) | 0.160 | |
| Umbilical cord gas acidaemia* | Unadjusted | 2.54 (1.58–4.06) | <0.001 |
| Adjusted | 1.84 (0.95–3.57) | 0.070 | |
| Admission to neonatal intensive care unit* | Unadjusted | 1.56 (1.21–2.01) | <0.001 |
| Adjusted | 1.60 (1.34–1.91) | <0.001 | |
| Neonatal trauma* | Unadjusted | 1.59 (1.18–2.15) | 0.003 |
| Not having a spontaneous vaginal birth* | Primiparas | 6.40 (3.96–10.36) | <0.001 |
| Multiparas | 9.81 (7.51–12.81) | <0.001 | |
| Combined | 6.28 (3.16–12.46) | <0.001 | |
| Instrumental vaginal birth* | Primiparas | 2.38 (1.87–3.04) | <0.001 |
| Multiparas | 7.86 (3.22–19.18 | <0.001 | |
| Combined | 2.72 (2.03–3.65) | <0.001 | |
| Forceps birth* | Combined | 6.20 (2.01–19.07) | 0.001 |
| Vacuum extraction* | Combined | 2.36 (1.88–2.97) | <0.001 |
| Oxytocin augmentation in labour* | Primiparas | 2.00 (1.78–2.25) | <0.001 |
| Multiparas | 1.42 (0.69–2.90) | 0.340 | |
| Combined | 2.23 (1.90–2.61) | <0.001 | |
| Adjusted | 1.44 (1.31–1.58) | <0.001 | |
| Neonatal mortality* | Unadjusted | 2.00 (1.65–2.42) | <0.001 |
| Adjusted | 1.49 (1.29–1.71) | <0.001 |
mean difference
Maternal outcomes
Birth type
Women giving birth in occiput posterior had a significantly increased risk of caesarean section, irrespective of parity (odds ratio: 6.74, P<0.001). They were also significantly more likely not to have a spontaneous vaginal birth (odds ratio: 6.28, P<0.001). When controlled for confounding factors, the mixed maternal group had an odds ratio of 2.72 (P<0.001) of instrumental vaginal birth.
Length of labour
The mean difference in total labour length was 0.85 hours (P=0.004) for the mixed group, with a mean difference in first-stage labour of 0.48 hours (P<0.001), and 0.55 hours for second-stage labour (P<0.001). This decreased to 0.46 hours (P<0.001) in adjusted analysis.
Other outcomes
Women giving birth in occiput posterior position were over three times as likely to experience a third or fourth degree perineal tear (odds ratio: 3.08, P<0.001), almost four times as likely to experience chorioamnionitis (odds ratio: 3.77, P<0.001) and more likely to receive oxytocin augmentation in labour (odds ratio: 1.44, P<0.001). None of the studies investigated postpartum infection as per definition (which requires two or more symptoms to be classified as postpartum infection), but two studies reported fever as a sign of infection in their results, and analysis found an odds ratio of 2.53 (P=0.009) with 0% heterogeneity. For primiparas, the mean difference of blood loss in the postpartum period was 0.28ml (P=0.004).
Newborn outcomes
When controlled for confounding factors, newborns had a mean difference of 0.24 (P<0.001) in Apgar score at 5 minutes, an odds ratio of 1.60 (P<0.001) of being admitted to the neonatal intensive care unit and an odds ratio of 1.49 (P<0.001) of experiencing morbidity.
Absolute risks
The absolute risk of experiencing a caesarean section was 26% (95% confidence interval: 8–43%) compared to women giving birth in occiput anterior position, while for severe perineal lacerations it was 10% (95% confidence interval: 6–14%) and for oxytocin augmentation, 15% (95% confidence interval: 13–17%). For newborns, the absolute risk of admission to the neonatal intensive care unit was 2% (95% confidence interval: 1–3%).
Discussion
This systematic review and meta-analysis explored birth outcomes to compare occiput posterior position with occiput anterior position across eight studies. The quality of the included studies, and challenges related to the observation and interpretation of perinatal outcomes, prevented certainty of some outcomes, but the high number of participants and effect sizes support the quality of evidence for other results. Bias, imprecision and inconsistency decreased the quality of evidence.
Among maternal outcomes with a moderate quality of evidence, women giving birth in persistent occiput posterior fetal position had a higher probability of caesarean section, in particular for multiparas, who also had a higher risk of instrumental vaginal birth. These women were also more likely to be given oxytocin augmentation in labour, and their newborns had a lower Apgar score at 5 minutes, as well as increased odds of being admitted to the neonatal intensive care unit and neonatal morbidity. The present review confirmed the high risk of caesarean section as mode of birth, a trend that has been widely reported and condemned by the authorities (Angolile et al, 2022). Manual rotation may be an effective technique for reducing the caesarean section rate in cases of an occiput posterior position during labour, but further training is required for midwives and obstetricians (Le Ray et al, 2007; Bertholdt et al, 2022; Allahbakhshi Nasabet al, 2023).
Perinatal outcomes in persistent occiput posterior births were less favourable than occiput anterior (Sizer and Nirmal, 2000; Fitzpatrick et al, 2001; Ponkey et al, 2003; Senécal et al, 2005; Cheng et al, 2006; Carseldine et al, 2013; Yagel et al, 2018). However, several factors must be considered. Most of the reviewed studies were retrospective observational cohorts, increasing heterogeneity among exposure. Heterogeneity was also increased by the different realities and clinical practices of each country of study. Several outcomes were reported using different measures, requiring transformation. Most of the data analysis relied on unadjusted data, leaving a gap in the interpretation of the true effects.
The quality of studies increased with time. The oldest studies failed to meet several reporting standards, but more recent studies made interpretation of the results less prone to bias. Studies reporting maternal outcomes presented more flaws, preventing clear interpretation of the results. Neonatal outcomes were reported by more recent studies, allowing for easier interpretation.
This is the first comprehensive systematic review to analyse the risks associated with persistent occiput fetal posterior position compared to anterior position. Despite a general understanding among practitioners that occiput posterior position increases adverse perinatal outcomes, the literature is vague on this topic. Previous reviews found that all adverse maternal outcomes had an association with occiput posterior position (Martino et al, 2007; Castel et al, 2019), and that results were more discordant for newborns (Castel et al, 2019). The results from the present systematic review confirm the risks for some maternal outcomes, but the results for neonatal outcomes reduce previous controversies.
Further research is required to understand the risks faced by women when their baby is malpositioned during labour. In addition, interventional studies should be promoted on the management and resolution of this dystocia. Where randomised clinical trials are not feasible, target trial emulations are a suitable method for answering causal questions without conducting experimental studies (Hernán and Robins, 2016).
Strengths and limitations
This systematic review had several strengths. The large sample sizes of the reviewed studies allowed for more precise estimates of treatment effect, and increased the generalisability of the results. Although most of the studies were retrospective, there were minimal missing data; this may be the result of the data collection and record-keeping methods implemented in high-income countries. Furthermore, the existence of several standardised perinatal outcome definitions, recognised at an international level, increased the chances of homogeneity of measurements across studies from different countries. Several outcomes were not prone to misclassification, and the design of retrospective cohort studies prevented observer bias. The increased magnitude of the effects of several outcomes raised the chances of true results, even when not adjusted for confounding, and the consistency of effects across all included studies decreased the possibility that the outcome results were generated by chance alone.
However, there were also limitations to the present review. All the included studies were observational cohorts, increasing the risk of bias and confounding effects, and promoting residual confounding. Most of the studies were retrospective, and the use of past medical records can be prone to potential errors (Garza et al, 2022). Measurement accuracy for the outcomes cannot be ascertained in retrospective studies, and measurements of the exposure are significantly prone to misclassification. Although digital vaginal examination is still the preferred method in most countries to ascertain fetal position during labour, the sensitivity of this tool is not high, and it is prone to errors: the occiput posterior position was reportedly not recognised in 50% of cases (Akmal et al, 2003; Dupuis et al, 2005). Misclassification of exposure was a severe limitation in the studies and, subsequently, for the present systematic review. Several studies failed to address confounding factors, and the inclusion of multiple study countries increased heterogeneity. Finally, the study populations were hospital based, excluding home births, increasing the risk of misclassification. A final note on the generalisability of the present review: while the studies included are set in high-income countries, there is a general lack of data about occiput posterior rate and management in developing countries, where the association between this labour malposition and perinatal outcomes remains uncertain.
Conclusions
Over time, there has been an interesting trend in studies of birth outcomes related to fetal malposition. Earlier studies focused on the woman during labour and the postpartum period, but later studies expanded to explore newborn outcomes and initial neonatal period. This alteration in focus reflects a change in clinical and public perspective.
With the improvement and increasing use of operative births, and improvement and development of neonatal care, there has been an increase in resolution of complications in labour through caesarean section, supported by improved neonatal care. Despite widespread condemnation of the increasing rate of caesarean section worldwide, the practice is not declining.
Persistent occiput posterior position is a common and well-noted fetal malposition, but despite its importance, there is a lack of literature exploring it. Current procedures most commonly used to resolve persistent occiput posterior position are operative vaginal and non-vaginal births, which increase the risk of negative maternal and neonatal outcomes. Maternal positions may have a significant impact on resolution of the dystocia, but the increased risks for mother and baby highlight the importance of exploring more moderate invasive procedures, such as manual rotation. The lack of research and training on manual rotation, which is a cost-effective manoeuvre, is experienced worldwide, and the gap should be filled with improvement of knowledge in this practice.
Appropriate research should be developed to expand understanding and awareness of manual rotation procedures, and to improve training and education on common fetal malpositions. Further research is required to understand the risks associated with fetal malposition, as well as how to manage and resolve this dystocia.
Key points
- Persistent occiput posterior fetal position is the most common fetal malposition during labour.
- Maternal and neonatal outcomes at birth are negatively affected by persistent occiput posterior fetal position.
- Manual rotation increases the rate of spontaneous vaginal birth, but more training is required.
- Target trial emulations provide a suitable method to estimate causal effect on perinatal outcomes when randomised clinical trials are not feasible.
CPD reflective questions
- What is the current practice in the management of persistent occiput posterior fetal position?
- Based on the evidence, what risk factors are associated with a high incidence of occiput posterior fetal position?
- Do you know how to perform the manual rotation maneuver?


