In September 2018, the North East Association of Directors of Public Health and both northeast local maternity systems identified the need for a dedicated resource to support seven ‘must do’ priorities. The resource was designed to reduce health inequalities and drive improvements in population health outcomes through maternity services. Partners acknowledged the complex systems that influence these outcomes (Rutter et al, 2017) and aimed to develop a programme that would maximise the impact of consistent, evidence-based, high-quality care. The programme's priorities included reducing smoking and alcohol use in pregnancy, increasing breastfeeding, supporting perinatal mental health, healthy weight, immunisations and the roll out of ‘making every contact count’.
A local maternity system prevention lead (a midwife and health visitor with public health experience) was appointed to deliver the programme, working collaboratively with heads of midwifery, among others. The programme lead was hosted by a local authority public health team and worked to strengthen and embed priority pathways across all local maternity settings. Audits were completed for each must do area, using National Institute for Health and Care Excellence (NICE, 2006; 2010a, b; 2014) guidance and evidence frameworks to establish a baseline. Events were held to share findings and recommendations widely. The team worked closely with many local and regional colleagues from across maternity, health visiting, local authority public health teams, regional offices for tobacco control (Fresh) and alcohol (Balance), National Institute of Healthcare Research, the North East and North Cumbria Applied Research Collaboration, maternity voices partnership, universities and voluntary, community and social enterprise organisations. In addition, they regularly shared their approach and learning with other networks, local maternity systems and national organisations.
In April 2021, further 2-year funding was approved by North East Commissioning Support, aligning the programme with the integrated care system's population health and prevention board. Now known as public health prevention in maternity, the programme maintained its focus on working in partnership to develop and embed robust regional pathways and practice innovations that support improving health and reducing health inequalities.
A steering group was established, including a lead director of public health on behalf of the northeast Association of Directors of Public Health, representatives from the local maternity system, Public Health England (now the Office for Health Improvement and Disparities), clinical commissioning groups, heads of midwifery, the North East and North Cumbria maternity clinical network and North East Commissioning Support.
The steering group developed the high-level programme priorities based on existing evidence and identified areas of practice that were most likely to reduce health inequalities and strengthen prevention. These priorities were then developed in partnership, including representation from professional partners and relevant client groups. The regional programme sought to ensure client views informed all developing pieces of work and complemented local engagement. Maternity voices partnerships provided a vital link and programme leads also conducted direct engagement. Maternity voices partnerships developed surveys on topics such as COVID-19 immunisations in pregnancy, that were distributed by members to a range of online groups (eg local pregnancy forums, local town interest groups, dads groups) as well as in person through partners distribution such as Haref (2023) (support for ethnically minoritised communities) to ensure appropriately diverse representation. The development of the tobacco dependency in pregnancy pathway included working directly with service users to ensure key messages would be well received by the targeted audience; an example of one such user, Serena, sharing her quit attempt can be found on the North Tees and Hartlepool NHS Foundation Trust YouTube page.
The public health prevention in maternity programme is delivered through a core team working closely with partners that include a range of frontline neonatal, maternity and community-based staff, public health teams and maternity voices partnerships.
The core team includes a public health prevention strategic manager for maternity, a public health practitioner and a maternal healthy weight and infant feeding coordinator. All team members have a clinical midwifery or midwifery and health visiting background, providing a strong understanding of working in the NHS system and clinical expertise.
Action
Programme priorities were refreshed in 2021, informed by local healthcare data on the scale of potential benefit and maternity system requirements, among other criteria. Objectives for each new priority area were developed through workshops and a stakeholder engagement event, which included regional leaders, clinical expertise, client representation and national experts.
Priorities and objectives
Tobacco dependency in pregnancy
- Implement high-quality in-house treatment for tobacco dependency as per the NHS (2019) long term plan
- Establish a regional NHS pregnancy e-voucher system
- Develop an enhanced smoking cessation support model to reduce relapse of tobacco use in the postnatal period
- Explore additional emotional and social support for women who are not able to quit.
Breastfeeding
- UNICEF baby friendly accreditation of maternity and neonatal services
- Embed the infant feeding pathway
- Support and evaluate small area pilots to increase breastfeeding continuation rates
- Tongue tie assessment and division service review.
Perinatal mental health
- Embed prevention elements of the perinatal mental health pathway
- Develop a pathway to include a 6-8 week statutory primary care review
- Continue to support maternal mental health service inequalities research.
Reproductive health and safe pregnancy spacing in the postnatal period
- Develop recommendations for preconception care and safe pregnancy spacing
- Improve pre-conceptive advice on tobacco dependency, alcohol use, positive mental health, postnatal contraception, nutrition and physical activity
- Develop a maternity contraception offer.
Maternal healthy weight
- Develop a set of recommendations for universal conversations relating to maternal healthy weight, physical activity and nutrition
- Promote and increase uptake of the Healthy Start voucher scheme
- Increase access to physical activity, targeting areas of deprivation
- Link local maternity services to free tier 2 weight management services, before, during and after pregnancy
- Consult with ethnic minority groups to be inclusive of specific needs.
Other areas
It was agreed that three previous programme areas had progressed sufficiently to be led at a local level with public health prevention in maternity programme input where required.
- Alcohol in pregnancy
- Immunisations in pregnancy
- Making every contact count.
Outputs and impact
The programme's leadership and collaboration with partners produced resources that, where embedded, enabled improvements in clinical practice and outcomes.
Tobacco dependency in pregnancy
The programme developed and led implementation of a robust pathway, where smoking status is established and referral for support and treatment is offered as standard. This was initially developed during the programme between September 2018 and April 2021. The pathway is based on an opt out model, in line with NICE (2021) guidance. A root cause analysis by senior system leaders (NHS chief executive, head of midwifery, the local maternity system, head of commissioning, head of social care, chief executive of commissioning, director of public health and public health consultant) assisted with changing the narrative from smoking as a lifestyle choice to the clinical treatment of nicotine dependency and tobacco-related harms. The work instigated the sign up of all local NHS chief executives to support embedding the pathway and provision of carbon monoxide monitoring equipment as essential clinical devices. Senior leaders continue to support their pledge to reduce smoking in pregnancy, making a clear contribution to the wider system's commitment to addressing tobacco-related harm, which remains a leading cause of health inequalities (Action on Smoking for Health, 2022).
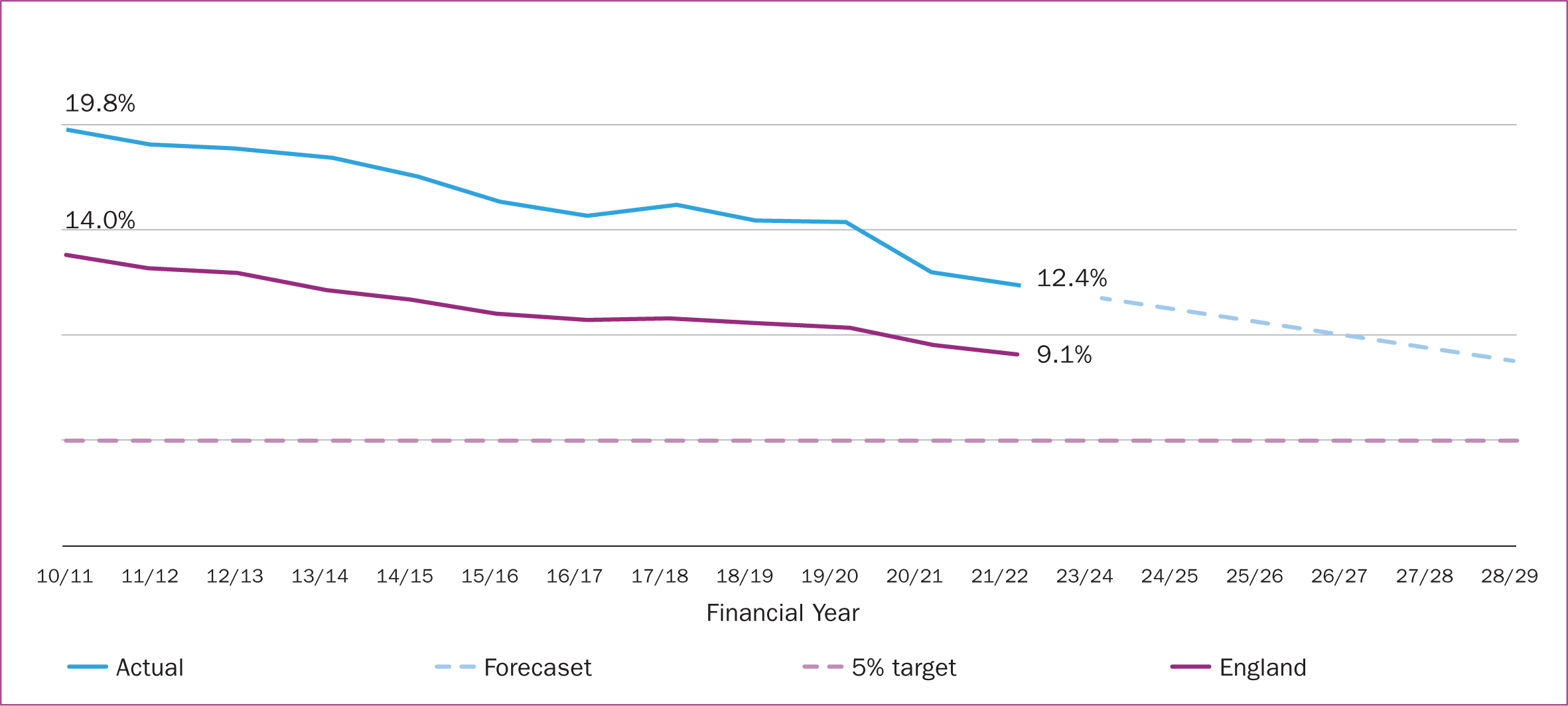
A 9-month pause in carbon monoxide monitoring, as a direct impact of the pandemic, significantly disrupted progress at a point where the new pathway was becoming establish as routine care. Despite this, the North East and North Cumbria Integrated Care System annual data show that smoking at time of birth rate reduced from 16.1% in 2017/18, at the inception of the programme, to 12.4%, compared to the 1.7% reduction seen for England (10.8% down to 9.1%) (NHS Digital, 2021). The programme has contributed to reducing this and associated health inequalities (Figure 1).
Breastfeeding
A regional strategy and pathway was developed for breastfeeding. The North East and North Cumbria Integrated Care System host the first integrated care system-wide breastfeeding guardian in the UK, ensuring accountability is achieved. There is continued engagement and progression with the UNICEF baby friendly initiative accreditation in almost all maternity and neonatal units and health visiting services. Table 1 demonstrates how implementing and achieving UNICEF baby friendly initiative accreditation and progressing to gold award has impacted breastfeeding prevalence at 6–8 weeks in the northeast.
Table 1. Comparison of breastfeeding prevalence pre- and post-services accreditation
| Local authority | Breastfeeding prevalence at 6–8 weeks (%) | |
|---|---|---|
| 2015–2016 (pre-accreditation) | 2021–2022 | |
| England | 43.7 | 49.3 (accredited) |
| Northeast (where data available) | 21.7 | 35.6 (accredited) |
| County Durham | 20.4 | Not validated (accredited to Gold Award) |
| Darlington | 13.0 | 35.1 |
| Gateshead | Not available | 40.7 |
| Hartlepool | Not available | 24.9 |
| Stockton on Tees | Not available | Not validated |
| Middlesborough | 18.0 | 33.9 (accredited to Gold Award) |
| Redcar and Cleveland | 19.0 | 31.5 (accredited to Gold Award) |
| Newcastle | 31.0 | 48.1 (accredited) |
| North Tyneside | 28.7 | 44.4 (accredited to Gold Award) |
| Northumberland | 27.5 | 42.0 (accredited to Gold Award) |
| South Tyneside | 17.3 | 28.2 |
| Sunderland | 20.8 | 27.6 |
| Cumbria (whole) | Not available | Not validated (accredited) |
Perinatal mental health
In partnership with the Perinatal Mental Health Clinical Network, a pathway and whole system approach was developed, focusing on universal care, identification, support to fathers and partners and special consideration of infant mental health. In response to feedback by the maternity voices partnership, a birth reflections best practice model was developed and embedded in all services (Scott, 2020). The evidence-based model ensures early follow up of birth trauma and identification of mental health support requirements, ensuring consistency, accessibility and clear lines of escalation to other services.
Reproductive health
A North East and North Cumbria Integrated Care System service review with recommendations for postnatal care, professional handover and contraception care has been written and shared. This review has a refined focus on preconceptual care in the postnatal period. Work to improve handover of care, access to pre-conceptive advice and the early postnatal contraception offer has begun, which is supported by contraception training for 180 midwives and health visitors.
Box 1.Feedback from system partners
- ‘Love the regional pathway's work and really appreciate the difficult negotiations that they have made…to get a better service for women and families’. NHS public health midwife
- ‘The usefulness, joint working and sharing of information has been incredible’. NHS England and NHS Improvement manager
- ‘I think this is a hugely valuable stream of work, which underpins wider public health. The team has been hugely influential in trying to standardise and promote good practice’. Maternity clinical educator
Maternal healthy weight
Best practice standards in relation to the pregnancy and postnatal period, alongside a supporting training package, have been developed and shared. A research proposal has been developed to explore active intervention and support during pregnancy, in order to further develop offers to pregnant women.
Alcohol
A pathway, screening tool and training package has been developed. An alcohol in pregnancy awareness campaign took place in winter 2022.
Immunisations
A best practice acute delivery model was developed and is being rolled out. A COVID-19 immunisations in pregnancy service review was conducted and key recommendations were shared with system partners including services, the local maternity and neonatal system, NHS England and NHS Improvement, the Office for Health Improvement and Disparities and through regional governance arrangements that were in place at the time.
Making every contact count
Developed in partnership with the North East and North Cumbria Integrated Care System making every contact count programme, specific training for the maternity and health visiting workforce was developed with access to a toolkit of resources.
Cross-thematic outputs
The team established the integrated care system public health midwives network, which provides a regular opportunity to share issues and best practice, consult on regional developments and receive updates and training from relevant organisations. The network members are able to share local barriers and explore solutions to programme implementation in a safe environment.
The team also worked with partners to develop a dashboard to improve access to maternity related data and enable insights that will help to refine targeted approaches to reducing health inequalities. The dashboard, which is still in its infancy, will enhance analytical capabilities by overlaying different sources of data at varied geographical levels, helping tailor support and services to local need.
Challenges
The programme has relied on successive short-term funding agreements. As such, the team was eager to maximise the impact of the programme and focused less on establishing and maintaining the programme's place in strategic and governance structures. On reflection, this led to some disconnect in the system at times and challenges that could have been avoided. These included work to develop mutually agreeable governance structures, increase ownership and enable integration of the programme into the local maternity and neonatal system.
A 2-year funding settlement, agreed as part of the developing integrated care system in April 2021, better enabled planning and provided a period of stability. However, establishing the programme outside of the local maternity system created a model of leadership that required ongoing management to ensure strategic alignment. Where possible, integrating the programme's future governance within the local maternity system is likely to best support the delivery of maternal and infant prevention priorities.
Reflections
Delivering a public health prevention programme in a complex maternity system and evolving NHS landscape has been challenging, rewarding and effective. The impact to date demonstrates that it is possible to add value and support improvements in this context, though there remains scope for development. The programme was strengthened by efforts to ensure appropriate representation and strategic support from steering group members (such as the local maternity system and vital links with heads of midwifery) and their organisations. Their influence helped to achieve operational change in local maternity services, while the programme remained accountable to the large emerging North East and North Cumbria Integrated Care System. Building on this engagement and mutual understanding will reduce barriers and increase the likelihood of future success.
Collaborating with partners to agree priorities that responded to local population and system need helped to develop relationships and shared ownership. The prioritisation exercise completed by the steering group, using agreed criteria, was a useful step in this process. The programme had most success where priorities mapped to greatest need, strongest evidence of effective intervention and were able to garner consistent support from senior leaders. As the programme is a regional ‘go to’ resource for maternity and the early postnatal period, opportunities to expand its scope often arise. Establishing clear programme priorities helped to manage this and define the role of the team in the context of wider partnership responsibilities.
While the team provided the capacity and expertise to develop high-quality resources, embedding the programme's priorities in routine maternity care depended on the support of others. When the approach worked best, colleagues advocated for the benefits of a public health prevention perspective and the importance of delivering this alongside other aspects of maternity care. Frontline practitioners remain at the heart of the programme. They have the passion and enthusiasm for change, although at times were working under difficult conditions. Staffing pressures, competing priorities and the impact of the pandemic all meant that the programme was not always able to progress as hoped. However, building effective relationships with partners and an understanding of their barriers has helped to maintain improvement where possible.
The programme has directly contributed to local maternity system deliverables, most recently the equity analysis and equity plan. Further consideration of the programme's strategic offer at a regional level, alongside support for implementing programme priorities, may be useful.
The programme's leadership has helped to raise the profile of preventing infant and maternal health inequalities as a system shared vision. It has contributed to improvements in population level outcomes, such as reductions in smoking at birth and, with its continuation, there is a real opportunity to further reduce associated health inequalities.
Conclusions
The commitment of the North East Association of Directors of Public Health and local maternity system colleagues across the North East and North Cumbria Integrated Care System has maintained a public health offer for maternity in the northeast since 2018. While funding and governance models have had to evolve, there is evidence that a focus on local need and establishing consistent evidence-based approaches can add value and improve the quality of preventative intervention at scale. The public health prevention in maternity team's role has been regularly communicated to ensure that existing services are supported by system-wide initiatives, efficiently overcoming barriers. The programme will continue to be evaluated to maximise its contribution, and governance will be reviewed during 2023/24.
Key points
- A new model of regional public health leadership was developed to complement the developing local maternity system.
- The programme was designed to reduce health inequalities and drive improvements in population health outcomes through maternity services.
- As part of a large, evolving and complex NHS system, the programme worked through significant challenges, such as complex leadership, governance models and prioritisation.
- There is clear evidence of the value added by the programme to the local system.
- Dedicated public health leadership helped raise the profile of infant and maternal health inequalities.
- The programme's collaboration with partners produced resources that, where embedded, enabled improvements in clinical practice and outcomes.
- Ongoing evaluation and work to embed a sustainable model of delivery remain important.


