Diabetes mellitus is an endocrine disorder in which insulin production or action is insufficient, resulting in hyperglycaemia. Insulin is produced in pancreatic beta (b) cells and is required for the uptake of glucose into cells, as well as the storage of glycogen, protein and fats. Thus, insufficient insulin action results in hyperglycaemia, and the breakdown of storage forms of fuel (glycogen, fats, and proteins) for use by the body's cells, due to lack of availability of glucose. There are three main types of diabetes (Table 1): type 1 diabetes is characterised by early age of onset, destruction of pancreatic b cells, and the need for therapeutic insulin. Type 2 is characterised by older age of onset, insulin resistance and insufficient insulin production to variable degrees, and is associated with obesity and a sedentary lifestyle. Gestational diabetes mellitus is seen only in pregnancy, typically in the third trimester, and it is thought to result from the metabolic changes brought on by pregnancy, along with an underlying predisposition to developing this condition (Crandall and Shamoon, 2015; American Diabetes Association (ADA), 2017; Rankin, 2017). This article will discuss the aetiology of gestational diabetes, how it is identified in pregnancy and controversies around this, adverse effects associated with it for the mother, fetus and child, and interventions aimed at preventing its development as well the associated adverse outcomes.
| Type 1 diabetes | Type 2 diabetes | Gestational diabetes | |
|---|---|---|---|
| Timing of onset | Usually during childhood or adolescence | Typically middle age or older, but increasingly seen at a younger age | During pregnancy, usually in the second or third trimester |
| Risk factors | Genetic susceptibility combined with an environmental trigger, such as viral infection (e.g. Cocksackie B4 virus), which is thought to trigger an autoimmune response | Genetic predisposition, obesity, age, sedentary lifestyle, previous gestational diabetes | Obesity, age, sedentary lifestyle, previous gestational diabetes |
| Pathophysiology | Autoimmune destruction of b cells, resulting eventually in a complete lack of insulin | Insulin resistance initially, usually combined with increasingly reduced insulin secretion | Insulin resistance in second half of pregnancy, combined with an underlying predisposition |
| Long-term effects | Vascular disease, which can cause kidney failure, blindness, stroke and death | Vascular disease, which can cause kidney failure, blindness, stroke and death | Type 2 diabetes and cardiovascular disease for the mother; obesity and type 2 diabetes for the child |
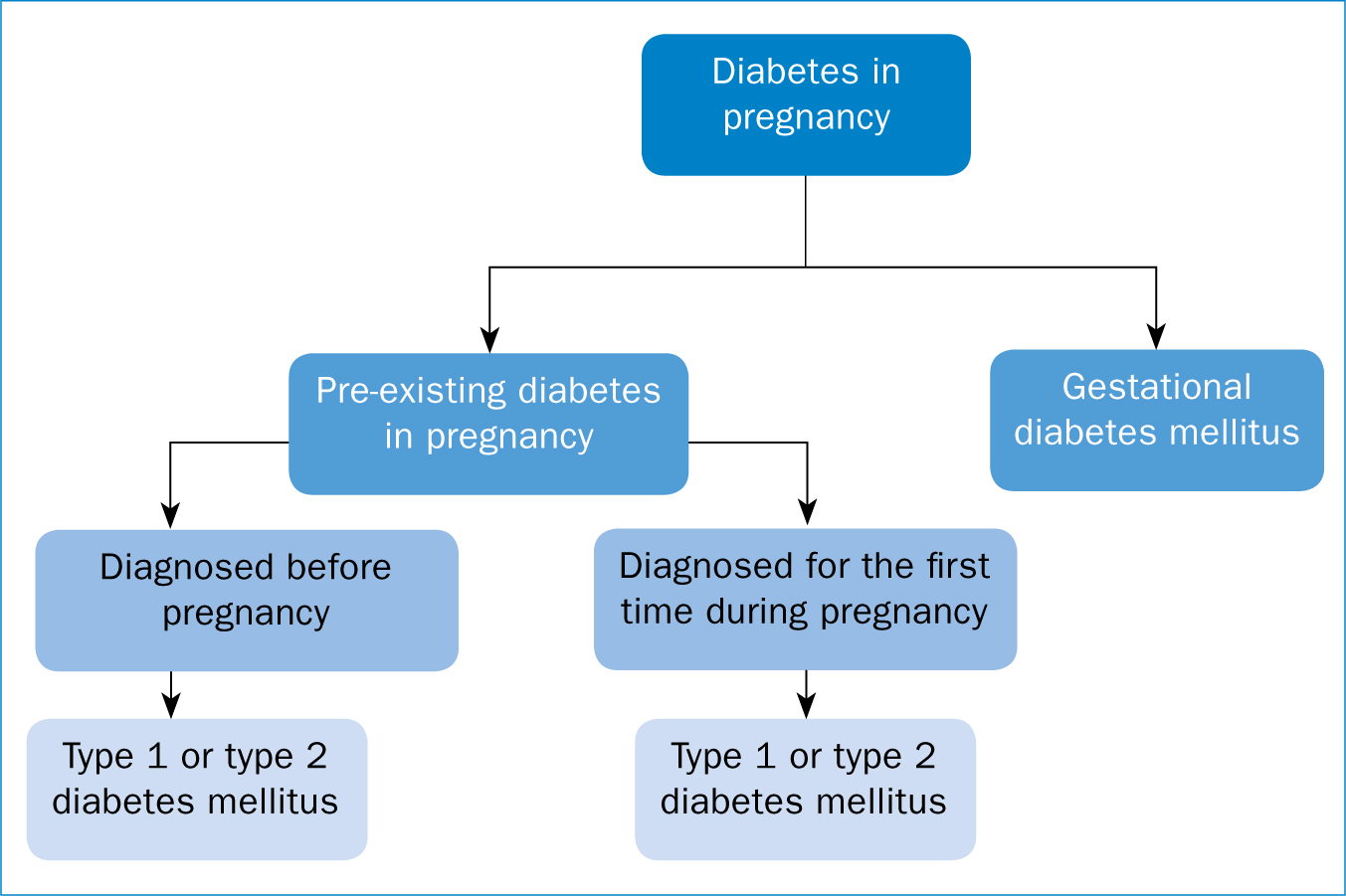
Gestational diabetes is diagnosed in the presence of hyperglycaemia that is recognised for the first time during pregnancy (Mirghani Dirar and Doupis, 2017). It is associated with an increased risk of several adverse outcomes for both the mother and fetus, which can be minimised with detection and management of the associated hyperglycaemia (Meek et al, 2015; Stewart and Murphy, 2015). It should, however, be distinguished from pre-existing diabetes (Figure 1), as this can be associated with additional adverse outcomes, including miscarriage and congenital anomalies, due to the presence of hyperglycaemia during conception, embryogenesis, and organogenesis (Hod et al, 2015; Gabbay-Benziv and Baschat, 2015; Blackburn, 2017). Diabetes affects around 5% of pregnancies, with most of these cases (87.5%) being gestational diabetes (National Institute for Health and Care Excellence (NICE), 2015), but whether hyperglycaemia is due to pre-existing diabetes or not can be difficult to ascertain, as most women are not screened for this condition before pregnancy (American College of Obstetricians and Gynecologists (ACOG), 2017). As gestational diabetes develops in the second half of pregnancy, screening for hyperglycaemia early in pregnancy could resolve this problem (Hod et al, 2015; Rankin, 2017).
The reported incidence of diabetes in pregnancy varies depending on the population studied, but it is estimated to affect between 5–7% of all pregnancies (Caissutti and Berghella, 2017; Piper et al, 2017). However, this figure is expected to rise due to the increasing incidence of obesity and type 2 diabetes, and the ever-younger onset of these, along with the increasing age of childbearing (ACOG, 2017). Therefore, more women are entering pregnancy with either pre-existing diabetes or with susceptibility to developing gestational diabetes (Hod et al, 2015). Along with its associated short-term effect, gestational diabetes imparts a huge burden on health at the population level, creating an amplifying intergenerational cycle of diabetes and obesity, which has the potential to significantly affect the epidemic of what has been labelled ‘diabesity’ (Monteiro et al, 2016). There is considerable controversy and disagreement around who, when, and how to screen for and diagnose gestational diabetes, with guidelines and methods used differing both between and within countries (Agarwal, 2015; Salmeen, 2016; Mirghani Dirar and Doupis, 2017; Kapur et al, 2018). Collaborative research is needed to determine the optimal methods for screening, diagnosis and management of gestational diabetes, and to provide a unified, evidence-driven approach that has the potential to halt the amplifying global cycle of diabetes and obesity.
Insulin and pregnancy
Diabetes results when there is insufficient insulin production and/or response to insulin to meet requirements. Insulin is secreted by pancreatic b cells in response to increasing blood glucose levels, and lowers blood glucose by stimulating the uptake of glucose into cells and promoting its storage (Figure 2). Thus, a deficiency in insulin secretion, an insufficient response to insulin, or a combination to various degrees of both will result in hyperglycaemia. Insulin also promotes the uptake and storage of other fuels, such as lipids and proteins. The first half of pregnancy (up to around 20 weeks) is associated with enhanced insulin sensitivity, promoting the storage of energy substrates for their use later in pregnancy and supporting the actions of insulin (Catalano and DeMouzon 2015; Blackburn, 2017) (Figure 2).

In the second and third trimesters, however, there is increasing insulin resistance. This is where, for the same level of insulin secretion, there is less response. For example, less glucose is taken up into cells, and the inhibitory effect on glycogen and lipid breakdown is reduced (various mechanisms for this are proposed but it likely most often results from post-receptor alterations that reduce the physiological response to the presence of circulating insulin). The aim of this is to allow mobilisation of glucose and amino acids for placental transfer to the fetus, while lipids are broken down and become the primary fuel for maternal use, due to the decreased maternal use of glucose (KC et al, 2015; Monteiro et al, 2016; Blackburn, 2017). Due to its catabolic effects on fuel metabolism, the second half of pregnancy is described as diabetogenic, as it somewhat resembles the underlying physiology of the diabetic state. Exactly what causes this increased insulin resistance is unclear, although the hormones human placental lactogen, human placental growth hormone, progesterone, and oestrogen are widely implicated (Baz et al, 2016; Blackburn, 2017; Burlina et al, 2017). As a result of this reduced uptake and use of glucose, there is a simultaneous and compensatory increase in insulin secretion by pancreatic b cells that keeps blood glucose at normal levels (Baz et al, 2016; Burlina et al, 2017).
Gestational diabetes
Gestational diabetes develops when the level of compensatory insulin secretion is insufficient to meet the level of insulin resistance, resulting in glucose intolerance and hyperglycaemia (Burlina et al, 2017). This can be due to diminished ability of pancreatic b cells to compensate for the level of insulin resistance, an enhanced level of insulin resistance, or a combination to various degrees of both (Powe et al, 2016). The manifestation of gestational diabetes is likely to be due to an underlying metabolic vulnerability that results in an inability to withstand the additional metabolic stress imposed by the diabetogenic state of pregnancy (Hod et al, 2015). This underlying vulnerability could be due to a single factor or a combination of factors including obesity or being overweight and genetic vulnerabilities that may also have already predisposed the woman to later type 2 diabetes (Hunt et al, 2014). It may therefore be that pregnancy tips an already delicate metabolic balance towards glucose intolerance and the development of gestational diabetes (Hod et al, 2015; Crandall and Shamoon, 2015). The effect of pregnancy on this underlying predisposition increases with advancing gestation (as insulin resistance increases), and the magnitude of the underlying condition will determine the timing of onset and severity of outcomes associated with it (Gabbay-Benziv and Baschat, 2015). Factors implicated in the pathophysiology of this increased sensitivity to the metabolic effects of pregnancy include genes involved in insulin-signalling and biochemical mediators produced as a result, or as part, of the underlying pathophysiology of obesity (Mirghani Dirar and Doupis, 2017). These include several adipocytokines (proteins that are released from adipocytes and alter various aspects of metabolism), including increased levels of leptin and TNF-a, and decreased levels of adiponectin (Al-Badri et al, 2015; KC et al, 2015; Mirghani Dirar and Doupis, 2017). Disparate pathophysiological mechanisms may be involved in gestational diabetes for different people, resulting in differing degrees of risk and therefore, potentially, in the need for varying degrees of intervention (Powe et al, 2016).
There is an increased risk of adverse pregnancy and fetal outcomes in the presence of gestational diabetes (Table 2). These include, for the mother, an increased risk of hypertensive disorders including pre-eclampsia, shoulder dystocia and caesarean delivery (Hod et al, 2015); and in the long-term, an increased risk of developing type 2 diabetes and cardiovascular disease, as well as gestational diabetes in future pregnancies (Phelan, 2016; Mirghani Dirar and Doupis, 2017). The increased risk of developing type 2 diabetes is not by any means insignificant, with up to 70% of women who have had gestational diabetes developing type 2 diabetes within 10 years postpartum (ACOG, 2017; Blackburn, 2017). For the fetus, short-term adverse outcomes include macrosomia, birth injury, neonatal hypoglycaemia and hyperbilirubinaemia (Hod et al, 2015); while long-term effects include an increased risk of obesity, type 2 diabetes, and for females, gestational diabetes later in life (Stewart and Murphy, 2015; Wang et al, 2018). The majority of these adverse effects are due to maternal hyperglycaemia, which causes fetal hyperinsulinaemia and macrosomia (Baz et al, 2016; Monteiro et al, 2016) (Figure 3).
| Maternal | Fetal/Infant | |
|---|---|---|
| Short term | Hypertensive disorders |
Macrosomia |
| Long term | Type 2 diabetes |
Obesity |

Screening for gestational diabetes
Interventions aimed at preventing hyperglycaemia—in the form of lifestyle modification, self-monitoring of blood glucose, and pharmacological therapy if required—can reduce the risk of adverse outcomes associated with gestational diabetes including macrosomia, shoulder dystocia, maternal hypertension and neonatal hyperglycaemia (Meek et al, 2015; Mirghani Dirar and Doupis, 2017). Therefore, it is essential that women with this condition are identified so that they can be appropriately treated, although there is a considerable and surprising lack of consensus around how best to achieve this. Methods used vary between and within countries, and recommendations differ depending on the advising body. Disparities and disagreements include: universal versus selective screening; how to selectively screen (using clinical risks or the 50g glucose challenge test); what risk factors to use to selectively screen and how to define these (e.g. what body mass index (BMI) defines risk); when to test; what type of test (75g or 100g glucose load), what sampling period to use; and what plasma glucose level defines diagnosis (Agarwal, 2015; Salmeen, 2016; Caissutti and Berghella, 2017; Kapur et al, 2018).
The aim of screening is to identify women who are defined to be at-risk, according to the parameters of the screening test used. NICE (2015) uses maternal clinical risk factors (Figure 4) to determine risk; however, there is a lack of agreement as to what risk factors should be included in this assessment as well as how to define these (Table 3). Furthermore, risk factors have only a moderate association with gestational diabetes, and only half of all women with gestational diabetes will have one or more risk factors (Hod et al, 2015; Kapur et al, 2017; Lindsay et al, 2017). It is therefore argued by many that screening using this method will miss a significant proportion of women who will consequently go untreated and may be at risk of adverse pregnancy outcome (Lindsay et al, 2017; Mirghani Dirar and Doupis, 2017; Piper et al, 2017; Kapur et al, 2018).

| Gestational diabetes risk factors | Risk factors used by NICE |
|---|---|
| Obesity/overweight |
BMI over 30kg/m2 |
NICE: National Institute for Health and Care Excellence
Given the increasing prevalence of obesity and diabetes, with the result that many more women are now entering pregnancy with pre-existing diabetes, the ADA (2017) recommends that women are screened for pre-existing diabetes and diagnostically tested if considered at-risk at their first antenatal visit. If this test is positive, this should be diagnosed as pre-gestational diabetes. If considered low-risk, women can be tested at 24 weeks using either a one-step or a two-step process (Figure 5). An alternative method is the universal screening of all pregnant woman at 24-28 weeks using the 75g oral glucose tolerance test (OGTT), which is the method recommended by the International Association for Diabetes in Pregnancy Study Group (IADPSG) (Metzger et al, 2010), the International Federation of Gynecology and Obstetrics (FIGO) (Hod et al, 2015), and the World Health Organization (WHO) (2013).

Further disparities lie in the number of abnormal blood glucose values required to define gestational diabetes, the blood glucose values used to define gestational diabetes, and the sampling time used, which can be 1, 2, or 3 hours (Bilous, 2015). The landmark Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study (Metzger et al, 2008) described the relationship between maternal plasma glucose levels and adverse outcomes, including pre-eclampsia, caesarean section, shoulder dystocia, neonatal hypoglycaemia, and hyperbilirubinaemia. The authors demonstrated that there is a linear relationship between plasma glucose and adverse outcomes, and that this relationship exists below levels used to define gestational diabetes, with no infliction- or break-point on which a diagnostic threshold can be based. Following this study, the IADPSG lowered their diagnostic threshold for gestational diabetes. The thresholds generated have been endorsed by WHO and adopted by ADA, but not ACOG or NICE (Table 4). The difficulty with this linear relationship is there is no obvious point on which to base a diagnostic threshold and this threshold may therefore depend upon the clinician's judgement around the relative importance of the risk and severity of adverse outcomes, and available resources (Salmeen, 2016). In fact, it has been suggested that there is no one-fits-all method, but that guidelines—such as those from FIGO, which recommend various options for screening and diagnosis depending on the country and situation in which they are to be implemented (Hod et al, 2015)—should be adapted to suit available resources (Salmeen, 2016).
| Advising body | Universal or selective | Diagnostic test | Fasting glucose (mmol/L) | 2-hr glucose (mmol/L) | No. of OGTT values for diagnosis |
|---|---|---|---|---|---|
| NICE | Selective based on clinical risk factors | 75g OGTT | 5.6 | 7.8 | 1 |
| IADPSG | Universal | 75g OGTT | 5.1 | 8.5 | 1 |
| ACOG (two-step) | Selective based on outcome of 50g GCT | 100g OGTT | 5.3 | 8.6 | 2 |
| WHO | Universal | 75g OGTT | 5.1 | 8.5 | 1 |
NICE: National Institute for Health and Care Excellence; IADPSG: International Association for Diabetes in Pregnancy Study Group; ACOG: American College of Obstetricians and Gynaecologists; WHO: World Health Organization; GCT: glucose challenge test; OGTT: oral glucose tolerance test
It is recognised that the universal method used by the IADPSG, as well as the lower diagnostic fasting plasma glucose levels, will result in significantly more women being diagnosed with gestational diabetes. This is likely to result in greater costs and add to the burden of time-constraints that many healthcare systems face (Bilous, 2015; Kapur et al, 2017). There are also concerns that the lower diagnostic threshold will add to the increasing medicalisation of pregnancy (more ultrasound scans, obstetric care, induction of labour or caesarean section) and that the psychological effect of this for the woman should be considered (Bilous, 2015; Salmeen, 2016). However, the economic and long-term cost of not treating certain low-risk women, or those who fall below the diagnostic net (whatever that might be) should also be considered; particularly given the long-term implications of increased risk of obesity and diabetes in children born to mothers with gestational diabetes. However, not every woman will require the same level of intervention, and this could be tailored to the woman's individual needs and preferences (Stewart and Murphy, 2015; Lindsay et al, 2017).
Intervention
That the nature of the intrauterine milieu has a strong and lasting effect on fetal programming is becoming increasingly evident (Wang et al, 2018), and this is no less the case for gestational diabetes. It has become increasingly clear that exposure to gestational diabetes in-utero, in addition to its short-term impact on the fetus, has a strong long-term impact in that it predisposes offspring to obesity and type 2 diabetes, and female offspring to future gestational diabetes (Monteiro, 2016; Burlina et al, 2017; Kapur et al, 2017; Wang et al, 2018). This creates an amplifying, intergenerational cycle, whereby increasing prevalence of diabetes and obesity increases the prevalence of these outcomes among offspring, and this effect is then perpetuated through future generations (Monteiro et al, 2016; Burlina et al, 2017; Kapur et al, 2017; Wang et al, 2018) (Figure 6). This is thought to be due to epigenetic modification (whereby gene expression is altered in a way that is heritable but also modifiable) of fetal genes as a result of the adverse intrauterine environment brought about by maternal hyperglycaemia (KC et al, 2015; Monteiro et al, 2016; Wang et al, 2018). Fetal genes potentially modified in this way include those encoding the adipocytokines previously mentioned, as well as genes involved in glucose and adipose homeostasis (Wang et al, 2018).

Despite the evidence showing that lifestyle intervention (promoting appropriate diet and exercise)— along with self-monitoring of blood glucose and medication if required—can reduce the risk of short-term adverse outcomes associated with gestational diabetes (Piper et al, 2017), there has been no clear evidence that these interventions can reduce the risk of developing the underlying gestational diabetes itself (Mirghani Dirar and Doupis, 2017; Piper et al, 2017). A recent Cochrane review (Shepherd et al, 2017) tentatively suggested that certain lifestyle interventions might be efficacious in reducing the risk of developing gestational diabetes; however, the authors could come to no strong conclusions. The power of studies carried out thus far to inform practice appears to be limited by methodological issues such as heterogeneity between studies regarding populations and interventions included, and small windows of opportunity within which to produce a significant effect (Phelan, 2016; Zhang et al, 2016; Shepherd et al, 2017). It is argued that the timing of diagnostic testing for gestational diabetes may be too late to allow interventions to exert their full effect, as the wheels for adverse outcomes may already be set in motion by this point, and there is also a limited time-frame for therapeutic intervention to take effect (Lindsay et al, 2017; Piper et al, 2017). In fact, the underlying metabolic sensitivities that predisposed women to gestational diabetes may have an effect early on in pregnancy, before gestational diabetes develops, perhaps even preconception. After all, many years of hyperglycaemia and potential type 2 diabetes can go unrecognised, but may be causing significant harm (Crandall and Shamoon, 2015). It may be that there are biomarkers, other than blood glucose, that may become evident and be tested for earlier, allowing more timely and thus potentially more efficacious intervention (Lindsay et al, 2017). Algorithms that use the level of various biomarkers and individual risk factors to calculate risk, similar to those developed to estimate risk for pre-eclampsia, have been suggested (Lindsay et al, 2017). This may allow risk stratification based on individual circumstances, rather than the dichotomous categorisation of care based on ambiguous methods of identification and diagnosis (Stewart and Murphy, 2015).
Lifestyle modifications have been shown to be effective in the prevention of future type 2 diabetes for mothers who have had gestational diabetes (Phelan, 2016; Mirghani Dirar and Doupis, 2017); and with up to 70% of women who develop type 2 diabetes within 10 years postpartum (ACOG, 2017; Blackburn, 2017), follow-up intervention is essential (Stewart and Murphy, 2016; Piper et al, 2017). It is unclear however, whether the intrauterine effect on future risk of obesity and diabetes for the child can be prevented through either lifestyle or pharmacological intervention during pregnancy (Monteiro et al, 2016; Shepherd et al, 2017). It may be that a longer intervention window is required, from preconception or early pregnancy through to the postpartum period and beyond, so that at-risk women can be identified and treated early on, and risks assessed and mitigated throughout pregnancy and into childhood for both mother and child (Phelan, 2016; Zhang et al, 2016; Kapur et al, 2018).
Conclusion
While the increased costs associated with more sensitive screening methods have been questioned, the inevitable financial and health burden associated with the rapidly increasing rates of obesity and type 2 diabetes should far outweigh this initial relatively insignificant financial input. There is convincing evidence that pregnancy represents a window of opportunity not only to improve the immediate and future health of both mother and child, but importantly, to slow the global epidemic of diabetes and obesity that, if left unchecked, could be perpetuated between generations. In fact, given the immediate and long-term effects of this condition, it is surprising that a unified, evidence-based approach to the identification and prevention of gestational diabetes has not yet been achieved. At the same time, not every woman who is diagnosed as having gestational diabetes will have the same level of risk, as evidenced by the linear relationship between plasma glucose and frequency of adverse outcome. In addition, underlying maternal factors are bound to impact upon this risk and it is perhaps time that protocols and interventions are modified to meet level of need, so that not every pregnancy affected by gestational diabetes needs the same level of financial input and medicalisation. Collaborative research is needed to address these issues in order to provide evidence-driven methods for screening and diagnosis, and to provide targeted intervention before, during, and after pregnancy, for both mother and child, in pursuance of a unified approach that will put an end to this deleterious cycle.

