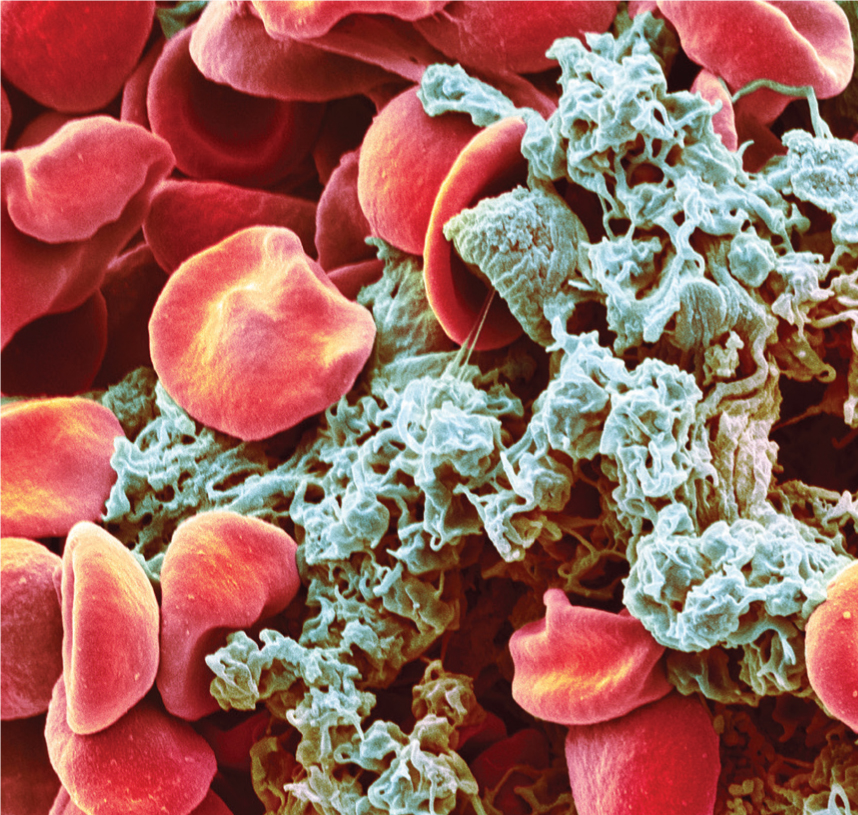
Platelets are ‘anucleate’ cell fragments that circulate in the blood and are critical for haemostasis (Figure 1). They usually exist in a quiescent state but upon vascular injury they become activated and adhere to damaged vascular walls in order to limit bleeding (Linden, 2013). Conversely, defective platelet activity is associated with increased bleeding. During pregnancy, platelets undergo several changes to offset the increased blood loss during birth and the immediate postpartum period.
Physiological changes during pregnancy
The usual range of platelet count is between 150–400 × 109/L, with a mean value around 260 × 109/L, although this can vary with age (Biino et al, 2013). Due to increased consumption in pregnancy, the platelet count falls, with statistically significant reductions noted in the third trimester. This fall is greater than reductions seen in both the first trimester and 8 weeks postpartum (Karlsson et al, 2014).
In contrast to a decreased platelet count, mean platelet volume (MPV) increases towards the third trimester of pregnancy (Han et al, 2014). Increased platelet volume is indicative of younger platelets, suggesting some increase in platelet turnover in pregnancy.
Platelet activity fluctuates throughout pregnancy and is a normal feature of pregnancy owing to the effects of complex coagulation factors such as thromboxane, collagen and other complex proteins. Platelet reactivity has been reported to decrease in the first trimester compared to non-pregnancy controls, but is more reactive towards the final trimester (Burke et al, 2013).
In most cases, changes in platelet activity during pregnancy are not associated with complications; however, there are some cases in which platelet activity induces a pathogenic response; for example, altered coagulation.
Coagulation changes during pregnancy
The changes in coagulation during pregnancy are well reported in respect of reducing the risk of excessive bleeding during birth (Hui et al, 2012).
The increased platelet activity affects coagulation, possibly due to increased levels of thrombin and soluble fibrin. This is compounded by elevated clot dispersal, evidenced by increased levels of degradation products such as serum D-dimers, assessed by serum sampling (Kawaguchi et al, 2013). D-dimers are the result of fibrinolysis, and consist of two cross-linked D fragments of fibrin. Although D-dimer levels increase during pregnancy, there are large fluctuations within normal pregnancies and they are not considered reliable measures to evaluate clinical outcomes (Hedengran et al, 2016).
The fine balance between formation and degradation of fibrin is important for normal haemostasis, as abnormal coagulation has been reported in conditions such as hypertensive states of pregnancy e.g. pre-eclampsia (Han et al, 2014). In spite of the normal changes in platelet function during pregnancy, it is useful to discuss specific platelet disorders that occur during pregnancy.
Thrombocytopaenia
Thrombocytopaenia is defined as a platelet count below 150 × 109/L (Gauer and Braun, 2012). There are various types of thrombocytopaenia and these may be associated with underlying medical complications of pregnancy such as: pre-eclampsia; haemolysis, elevated liver enzymes and low platelet (HELLP) syndrome; and thrombotic thrombocytopaenic purpura.
The types and frequency of thrombocytopaenia are illustrated in Table 1.
| Type of thrombocytopaenia | Percentage of cases of thrombocytopaenia in pregnancy |
|---|---|
| Gestational thrombocytopaenia | 70–80% |
| Immune thrombocytopaenia | 1–11% |
| Pre-eclampsia | 15–20% |
| Haemolysis, elevated liver enzymes, low platelets syndrome | < 1% |
| Thrombotic thrombocytopaenic purpura | < 1% |
Gestational thrombocytopaenia
Gestational thrombocytopaenia is defined as ‘mild thrombocytopaenia occurring during the third trimester with spontaneous resolution postpartum’ (Boehlen, 2006: 72) and affects up to 10% of pregnancies (McCrae, 2010). It is reported that gestational thrombocytopaenia is caused by increased platelet clearance due to physiological haemodilution during pregnancy. Owing to the lack of specific tests available, gestational thrombocytopaenia is currently diagnosed by exclusion (Gernsheimer et al, 2013; Kasai et al, 2015).
Gestational thrombocytopaenia is usually mild, with counts of 130–150 × 109/L recorded in two thirds of cases (Gernsheimer et al, 2013), although this value may drop further without adverse complications. Overall, there are no negative effects to the fetus (Gernsheimer et al, 2013; Townsley, 2013); however, gestational thrombocytopaenia is associated with increased rates of placental abruption (Parnas et al, 2006). Therefore, even mild gestational thrombocytopaenia has the potential for serious complications.
Immune thrombocytopaenia
A further condition affecting pregnancy is known as immune thrombocytopaenia, which is described as ‘isolated thrombocytopaenia with no clinically apparent associated conditions or other causes of thrombocytopaenia’ (George, 2009: 759). It has an 11% incidence and is due to an autoimmune reaction against platelets, where autoantibodies trigger platelet destruction (McMillan, 2009).
Two thirds of women with immune thrombocytopaenia during pregnancy do not require treatment, and bleeding is uncommon (Townsley, 2013). The woman's platelet count usually recovers following birth (Kasai et al, 2015). Where treatment is required, this entails either corticosteroids or intravenous immunoglobulin (Townsley, 2013). Treatment to maintain platelet count may be required immediately prior to labour, either to prevent haemorrhage or administer spinal anaesthesia. Thrombocytopaenia can be a contraindication for spinal anaesthesia; however, counts of 80 × 109/L are reported as safe providing there are no other overt coagulation defects or risk factors (van Veen et al, 2010; Gernsheimer et al, 2013). This condition is also diagnosed by exclusion (Townsley, 2013), making it difficult to distinguish from gestational thrombocytopaenia. As a general rule, a declining platelet count below 100 × 109/L in the first trimester indicates immune thrombocytopaenia (Gernsheimer et al, 2013). Mild symptoms, such as bruising, may occur; mucosal or cutaneous bleeding may be evident in some cases and platelet counts may fall below 30 × 109/L in 22% of pregnancies with immune thrombocytopaenia (Loustau et al, 2014).
Thrombotic thrombocytopaenic purpura
Thrombotic thrombocytopaenic purpura (TTP) is a rare but serious platelet disorder affecting approximately 6/1 000 000 people; 25% of cases occur in pregnancy. It is characterised by red blood cell destruction, thrombocytopaenia, kidney dysfunction, fever and neurological symptoms such as headache, although in 35% of cases neurological symptoms are not apparent (Scully et al, 2012). Thrombocytopaenia occurs as the platelets are consumed as small thrombi form in the microvasculature damaging the kidneys and other organs (Scully et al, 2012). TTP once had survival rates as low as 10%, but the introduction of plasma exchange treatment has greatly improved survival to 80% (Hovinga et al, 2010).
‘Detection of platelet changes may help in the early detection of hypertensive states of pregnancy and, in pre-eclampsia, the mean platelet volume is increased compared to normal pregnancy’
It is reported that pregnancy increases the risk of TTP by triggering the production of placental antibodies against ADAMTS13, an enzyme that degrades a protein involved in blood clotting (Gerth et al, 2009). Indeed, women with ADAMTS13 activity less than 25% have three times the risk of developing TTP and the presence of autoantibodies is associated with a 4.1-fold increased risk of miscarriage. Crucially, ADAMTS13 immunity may be present for several years after recovery from TTP, although its significance in relapse has yet to be established (Ferrari et al, 2014).
Most pregnancies with TTP conclude with normal births; however, the disorder can increase the risk of developing pre-eclampsia in subsequent pregnancies (Jiang et al, 2014). Therefore, monitoring ADAMTS13 activity may help in the diagnosis of TTP and facilitate detection before the onset of symptoms (Scully et al, 2012).
Pre-eclampsia
Pre-eclampsia is a severe, multisystem disorder characterised by hypertension and proteinuria, and is a major cause of global pregnancy-related mortality, affecting up to 8% of all pregnancies (Dundar et al, 2008). In the UK, the mortality rate is 0.42/100 000 maternities (Knight et al, 2014). Associated risk factors include obesity, smoking, primigravid status and history of hypertension (Shamsi et al, 2013). Clinical risks include cerebral haemorrhage, placental abruption, end organ failure and, rarely, stroke or death (Knight et al, 2014). By far the most common cause of maternal death from pre-eclampsia is intracranial haemorrhage (Cantwell et al, 2011). Pre-eclampsia also raises the risk of cardiovascular problems later in life (Ahmed et al, 2014), possibly associated with the increased platelet activity. Overall, it is the peripheral vasoconstriction that is thought to lead to the hypertension associated with pre-eclampsia.
Fetal growth restriction and preterm birth are significant dangers to the neonate (Lin et al, 2015).
There are several proposed mechanisms behind the cause of pre-eclampsia, and these may differ between women. Although the pathogenesis is not fully known, it is reported that a disrupted immune/inflammatory response or poor placentation are primary causes of pre-eclampsia. During normal placentation, the maternal spiral arteries undergo significant remodelling following invasion by placental cytotrophoblasts; however, this process is disrupted in pre-eclampsia (Fisher, 2015). During placental development, there is significant angiogenesis (formation of new blood vessels). An imbalance between pro- and anti-angiogenic factors may affect utero-placental angiogenesis leading to pre-eclampsia (Noori et al, 2010). The reduced blood flow to the placenta can trigger a release of circulating factors such as inflammatory cytokines. Animal models of this have demonstrated signs resembling pre-eclampsia e.g. hypertension and proteinuria (Mutter and Karumanchi, 2008). Pre-eclampsia is also associated with endothelial dysfunction and reduced release of nitric oxide and increased production of reactive oxygen species (Matsubara et al, 2015). Release of a molecule called TxA2 can increase during pre-eclampsia, which can lead to vasoconstriction and increased platelet activity (Ahmed et al, 2014).
Detection of platelet changes may help in the early detection of hypertensive states of pregnancy and, in pre-eclampsia, the MPV is increased compared to normal pregnancy (Dundar et al, 2008). Importantly, MPV increases up to 4–6 weeks before the characteristic increase in blood pressure (Dadhich et al, 2012). During weeks 24–28, women with a MPV over 8.5 fL are twice as likely to develop pre-eclampsia (Dundar et al, 2008). Monitoring platelets could, therefore, offer an earlier opportunity to identify pre-eclampsia (Özdemirci et al, 2016). However, it should be noted that the sensitivity and specificity of MPV as a precursor for pre-eclampsia is less than 80% (Özdemirci et al, 2016). Standardised reporting protocols may help improve consistency and confirm the reliability of using MPV to help detect the onset of pre-eclampsia and, although current parameters alone are not reliable, they may help to identify women who are more likely to develop pre-eclampsia later in their pregnancy. Compounding the imperfections in laboratory methods, late presentation of pre-eclampsia further frustrates accurate prediction of the disease. It is reported that other methods for diagnosing pre-eclampsia would be helpful (Sibai and Stella, 2009). In this respect, a state of enhanced platelet activation has been reported in some pre-eclampsia patients; however, reliable biomarkers for diagnosis are yet to be established (Freitas et al, 2014).
Haemolysis, elevated liver enzymes, low platelets (HELLP) syndrome
This syndrome is a severe form of pre-eclampsia characterised by haemolysis, elevated liver enzymes and low platelets (Kirkpatrick, 2010). It occurs in 0.9% of all pregnancies; however, up to 10–20% of patients with severe pre-eclampsia also develop HELLP syndrome. The peak onset is between 27–37 weeks, but it may occur up to 48 hours post-birth (Haram et al, 2009). In the last Confidential Enquiry into Maternal Deaths (Knight et al, 2014), nine women per 100 000 births died and perinatal mortality was reported at 14.3%. Neonates are also more likely to require intensive care and respiratory ventilation (Turgut et al, 2010).
The syndrome is diagnosed using the Tennessee classification system i.e. haemolysis, lactate dehydrogenase (LDH) levels above 600 U/L, aspartate aminotransferase (AST) above 70 U/L, and thrombocytopaenia below 100 × 109/L, and all three signs must be displayed. Further, the Mississippi system also classifies HELLP into three types of severity, with the inclusion of alanine aminotransferase levels (Haram et al, 2009).
Overall, HELLP syndrome is a progressive condition with potentially serious complications, such as disseminated intravascular coagulation (DIC) and ruptured liver haematoma. The risk of recurrence in a subsequent pregnancy is 12.8% for HELLP, 16.2% for pre-eclampsia and 14.2% for gestational hypertension (Leeners et al, 2011).
Additionally, development of early HELLP syndrome is associated with disordered coagulation through higher fibronectin and D-dimer levels and reduced antithrombin. It is reported that monitoring plasma fibronectin or coagulation inhibitors could help indicate the early onset of HELLP (Haram et al, 2009).
Von Willebrand factor
The endothelial activation associated with HELLP syndrome may lead to an increase in the release of the platelet activating protein, von Willebrand factor (vWF). This is increased in HELLP syndrome i.e. 1.6–2 times that of normal or pre-eclampsia pregnancies, respectively. Compounding this is a reduction in a protein that usually degrades vWF, thereby limiting platelet activity, favouring platelet activation and depleting platelet levels; hence, playing an important role in the formation of intravascular thrombi seen in HELLP syndrome (Pourrat et al, 2013). In spite of counterbalances, continuous platelet activation exhausts inhibitory mechanisms further contributing to DIC (Abildgaard and Heimdal, 2013) and the characteristic end organ dysfunction (Haram et al, 2009).
The endothelial dysfunction of pre-eclampsia and HELLP syndrome contribute to platelet activation; specifically, cytokines released from activated endothelial cells promote platelet activation and inflammatory changes. Further, platelets demonstrate increased expression of proteins causing inflammation in both pre-eclampsia and HELLP, thus potentiating endothelial dysfunction and inflammation, further promoting platelet activation (Azzam et al, 2013).
Treatment for HELLP can involve maternal platelet transfusions to increase platelet count, but corticosteroid therapy promotes platelets and is also more cost-effective and associated with a shorter hospital stay. However, corticosteroid treatment is not associated with improved maternal mortality or morbidity (Mao and Chen, 2015).
Management of platelet activation with platelet or coagulation inhibitors may help prevent low platelets and, more importantly, limit the intravascular thrombi formation (Hulstein et al, 2006).
The only effective curtailment of HELLP syndrome is birth of the fetus, and if early birth is required this is associated with higher perinatal mortality. In addition, 40% of neonates will develop respiratory distress syndrome, although corticosteroids can promote lung maturation (Haram et al, 2009).
Conclusions
Normally, the physiology of pregnancy is well tolerated by most women, without any deleterious effects. However, for some women, the physiological changes to platelets can contribute to the pathogenesis of important pregnancy-related conditions. Moreover, normal platelet homeostasis can be disrupted by endothelial dysfunction causing the release of inflammatory mediators, further potentiating platelet activity. Such disruption may exacerbate underlying conditions, leading to potentially serious complications that pose significant risk to both the woman and fetus.
Importantly, platelets demonstrate changes during the development of some conditions that may precede the onset of signs/symptoms. Hence, an understanding platelet physiology in pregnancy may increase awareness of potential complications necessitating appropriate referral, thus facilitating an improved diagnosis.

