The continual increase in caesarean section rates in the UK has been recognised as a public health issue because of a lack of evidence that caesarean section generates better (or at least equitable) mother–infant outcomes compared to vaginal delivery (D'Souza and Arulkumaran, 2013; D'Souza, 2013; Wise, 2018). The World Health Organization emphasises that caesarean section rates over 15%, such as in the UK where the rate is currently 26.2%, is indicative of unnecessary and therefore unethical surgical intervention (Betrán et al, 2016; Wise, 2018).
The National Institute for Health and Care Excellence (NICE, 2013) guidelines state informed choice/consent is the pinnacle in enabling women to act as equal partners in deciding their mode of birth in a clinical environment. Informed choice is achieved by maternity care providers supplying women with impartial, evidence-based information (D'Souza, 2013; NICE, 2013; Moore, 2016). The long-term benefits of shared decision making in obstetrics are widely recognised and include increased equity in care, decreased litigation because of improved patient satisfaction and better patient outcomes resulting in reduced post-care complications (Gee and Corry, 2012). Results from international studies identify that UK providers score highly in indicators of supporting women's rights to caesarean section as an informed choice (Habiba et al, 2006; Betrán et al, 2016). However, shared decision making and informed choice are misunderstood by healthcare providers and are mostly comprised of a shallow process of decanting knowledge to lay persons in order to obtain a consent signature (Begley et al, 2019).
Overall, there is a current lack of understanding regarding women's decision making with respect to caesarean section and if women are genuinely undergoing caesarean section as part of an informed procedure. The present review aimed to shed light on women's decision making experiences of scheduled and unscheduled caesarean section in the UK, by exploring women's narratives. The goals of this systematic review were two-fold; first, to systematically synthesise qualitative data surrounding women's viewpoints and experiences of shared decision making in undergoing caesarean section surgery, both scheduled and unscheduled. Second, to investigate women's satisfaction and needs associated with their decision-making process for caesarean section as an informed procedure.
Methods
The following databases were systematically searched for peer-reviewed, full text, primary research articles published between 1990 and 2020:
- MEDLINE via EBSCO (MEDLINE, CINAHL, PsychNFO, AMED)
- EMBASE via OVID
- Maternity and Infant Care Database (MIDIRS via OVID)
- Scopus
- Wiley Online Library.
In addition, a grey literature search was conducted by searching Google Scholar Ethos as well as the reference sections of the included studies. The first author developed an initial search strategy consisting of a combination of keywords and MeSH terms. The search strategy was adapted for use in the different databases and was configured according to the Population, Intervention, Comparison, Outcome (PICO) framework surrounding six concepts that were connected using appropriate Boolean operators and truncation:
- Cesarean OR Caesarean Section
- Mothers OR Postnatal OR women etc
- Decision-making OR Authoritative Knowledge etc
- Psychosocial outcomes OR Satisfaction etc
- UK
- Qualitative method OR interview etc.
Only English language journals published after 1990 were included for synthesis. The lower limitation was set to 1990, as the patient-centred care approach was first adapted in the UK in the 90s stemming from the US Chronic Care Model (The Health Foundation, 2014). Maternal choice in obstetric care policies were first implemented in the UK in 1993 (Paranjothy, 2004; Kingdon et al, 2009).
Qualitative studies including women who had given birth via caesarean section delivery in a UK healthcare facility were considered for analysis. Mixed methods studies were also included if findings from the qualitative component could be extracted. There were no restrictions on caesarean section intervention type; however, it was decided that studies on pregnant women's decision making regarding mode of birth with a focus on vaginal birth after a previous caesarean diverted from the review question and were therefore excluded. In addition, studies focusing on the views or experiences of the non-maternity population (eg partner, health professional) were excluded. Studies were selected for inclusion via a purpose-designed data extraction form.
The PRISMA flowchart shown in Figure 1 was followed in processing and recording study selection outcomes (Moher et al, 2009). The first stage consisted of the first author reviewing all studies at title and abstract level, the second author reviewed 10% of the studies in order to check for consistency in approach of inclusion and exclusion criteria. Though the authors acknowledge full dual-reviewer screening as best practice, single-reviewer screening is recognised as an acceptable method when there are time limitations (Cochrane Information Retrieval Methods Group, 2019). Following this, the first and second author independently reviewed all the studies identified for full text review. All discrepancies were resolved via consensus.
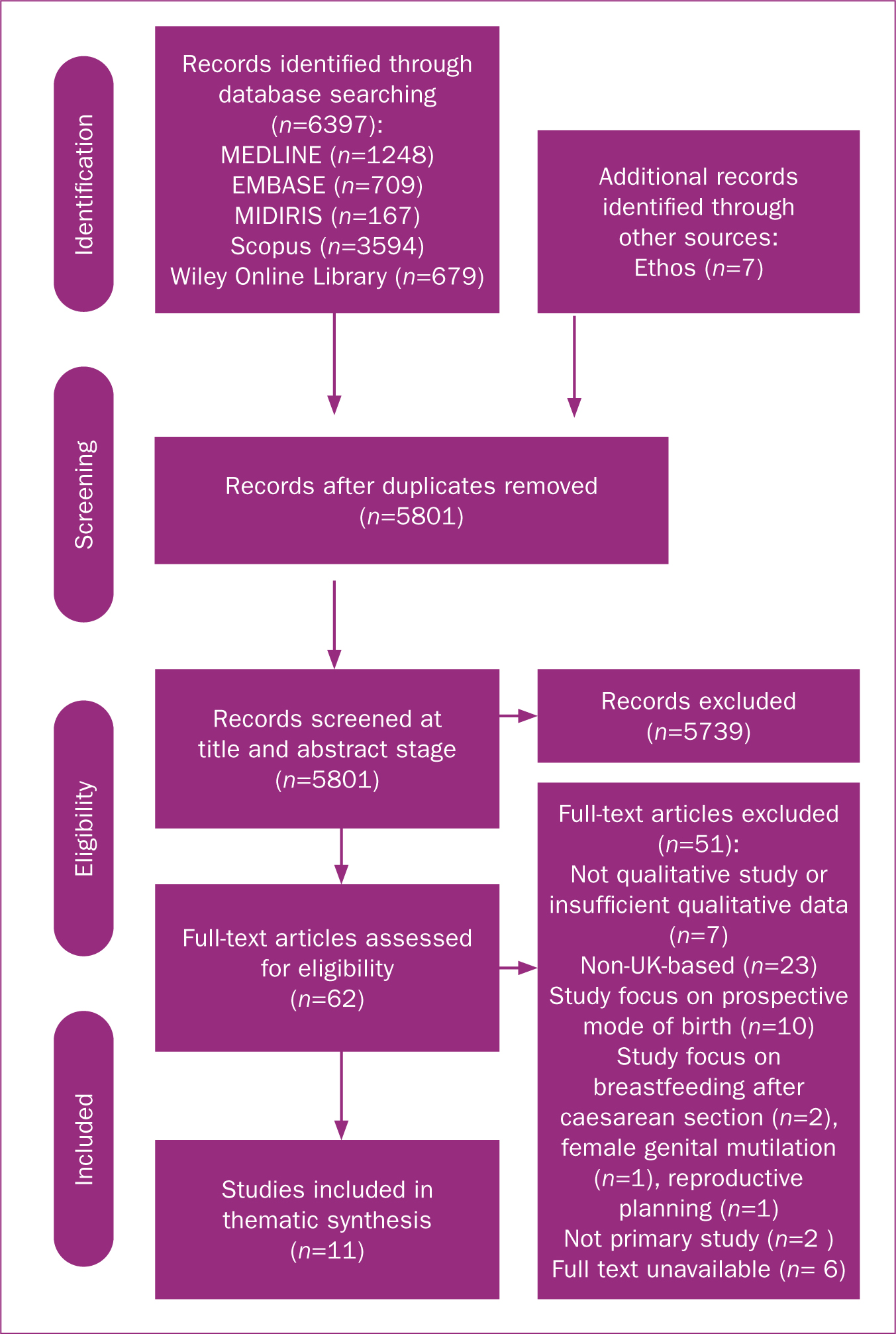 Figure 1. PRISMA flow diagram
Figure 1. PRISMA flow diagram
Thematic synthesis was employed to amalgamate descriptive themes, so as to arrive at a novel interpretation of the existing literature surrounding women's experiences of caesarean section. Three steps were followed in using thematic synthesis to tabulate qualitative data. This process consisted of:
- Extrapolation of primary qualitative data obtained from the findings sections into the NVivo 12 software, followed by line-by-line coding of free codes that emerge from the text
- Aggregating of the free codes into related areas of descriptive themes using an inductive process of cross-comparison until no new concepts could be coded into pre-existing ones
- Development of analytical themes or higher-order themes that go beyond primary results in offering new understanding of the primary results.
The aim to investigate caesarean section as informed patient choice dovetails with the epistemological positioning of thematic synthesis in investigating viewpoints and experiences in order to answer questions regarding suitability and acceptability of an intervention (Thomas and Harden, 2008).
Results
The search strategy yielded 6404 studies for potential inclusion. Following removal of 603 duplicates and elimination of 5739 studies at title and abstract stage, 62 studies were identified for full text review, resulting in 11 studies that were included in the final analysis (Figure 1).
Studies included the results from 242 multiparous and primiparous women that were interviewed individually or in focus groups (Murphy et al, 2003; York et al, 2005; Baston, 2006; Fenwick et al, 2009; Tully and Ball, 2013; Mason, 2015; Kenyon et al, 2016; van Griensven et al, 2016; Weckesser et al, 2019), as well as the open-ended survey responses of 1203 women (Porter et al, 2007; Redshaw and Hockley, 2010).
Nearly half of the studies (n=5) were mixed method design (Baston, 2006; van Griensven et al, 2016) or part of a larger quantitative study (Murphy et al, 2003; Porter et al, 2007; Redshaw and Hockley, 2010).
Qualitative data components were analysed using thematic analysis (Murphy et al, 2003; York et al, 2005; Weckesser et al, 2019), content analysis (Porter et al, 2007; Redshaw and Hockley, 2010; Tully and Ball, 2013), narrative analysis (Mason, 2019), framework analysis (Kenyon et al, 2016; van Griensven et al, 2016) and grounded theory (Baston, 2006; Fenwick et al, 2009).
Data were collected between 1 day and 20 years postpartum, and only one study considered recollection bias in their study design by piloting the study on women who had given birth more recently (Murphy et al, 2003).
Studies that reported participant ethnicity (n=7) identified that 75% or more of participants were white (Murphy et al, 2003; Fenwick et al, 2009; Redshaw and Hockley, 2010; Tully and Ball, 2013; Kenyon et al, 2016), or white British (York et al, 2005; Weckesser et al, 2019). Most studies that did not publish participants' ethnicities discussed lack of representativeness as a limitation. (Baston, 2006; Mason, 2015; van Griensven et al, 2016). Table 1 shows a summary of included studies.
Table 1. Sumary of included studies
| Study locality | Participants | Study aims | Data collection | Methodology | Key themes/findings |
|---|---|---|---|---|---|
| Boston (2006), north England | Women, unscheduled caesarean section, aged 21–34 years, n=21 | Explore women's perceptions/experiences of sequelae and care in emergency caesarean | Semi-structured interviews, 4 years postpartum | Grounded theory | Relationships with caregivers key to appraise birth and decision-making process. Themes: emotional wellbeing, women's perception of staff, ‘intelligent guardianship’ |
| Fenwick et al (2009), southwest England | Primi- and multiparous women, scheduled and unscheduled caesarean section, aged 25–35 years (n=21) | Explore women's experiences of caesarean section | Unstructured interviews conducted 7–32 weeks, with one at 18 months, postnatal | Grounded theory | Four key themes linked by core theme ‘achieving normality’: expectations and reality, being in control, feelings of failure as a woman, feeling different |
| Van Griensven et al (2016), southeast England | Women, scheduled and unscheduled caesarean section (n=19) | Explore impact of scar problems and perceived needs, with aim of informing healthcare | Semi-structured interviews conducted via phone 11–35 months postpartum | Framework analysis | Improved pre-operation preparation and educating are key. Themes: persistent scar problems, professional help for scar problems, preparation for and recovery from caesarean |
| Kenyon et al (2016), Birmingham, England | Primi- and multiparous women, scheduled caesarean section (n=15) | Investigate women's experiences of requesting caesarean section and healthcare systems with wider aim of improving care pathway | Semi-structured interviews (n=15) and workshops (n=8), which included maternity healthcare professionals. Timeframe not mentioned | Framework analysis | ‘Touchpoints’ from workshops: information available, delayed decision making, need to repeatedly defend decision. ‘Touchpoints’ from joint workshops: making request to community midwife, consultant obstetrician or consultant midwife, mental health services, antenatal care, postnatal care in community |
| Mason (2015), south England and Midlands | Primiparous women, scheduled caesarean section (n=8) | Explore how caesarean section births are understood and constructed by women having first baby via caesarean | Semi-structured interviews conducted 4 weeks–1 year postpartum | Narrative analysis, ‘the listening guide’ method | Decision making to undergo caesarean and acceptance of decision evolved around interpersonal processing and negotiating surrounding ‘good mother’ ideology. Themes: self-efficacy and fatalisms |
| Murphy et al (2003), England | Primi- and multiparous women, scheduled and unscheduled caesarean section, aged 21–40 years (n=12) | Explore the views of women regarding the impact of operative delivery in the second stage of labour | Semi-structured interviews conducted up to 2 years postpartum | Thematic analysis | Unprepared for operative intervention and recovery period. Themes: preparation of delivery and usefulness of birth plan, understanding of indications for operative delivery, need for de-brief and medical review, future pregnancy and delivery |
| Porter at al (2007), Aberdeen, Scotland | Women, scheduled and unscheduled caesarean section. Mean age 27.1 years (n=521) | Explore factors reported as ‘distressing’ regarding birth, aimed to understand women's needs | Analysis of open-ended questions from survey conducted 5–20 years postpartum, average 14 years after birth | Content analysis | Negative effect of failed labour, delayed recovery and emergency situation compacted by lack of information and communication. Themes: before, during and after birth, psychological and general issues, women's overall concerns |
| Redshaw et al (2010), England | Women, scheduled and unscheduled caesarean section, aged 16–40+ years. More than half fell within 30–39 age category (n=682) | Understand how women perceive care surrounding caesarean | Analysis of open ended questions from survey at 3 months postpartum | Thematic content analysis | Helplessness and disempowerment are compounded by recovery. Themes: feelings, being heard, managing communications, illusion of choice, how it might have been different, ‘just another new mother’, wounds and hurt feelings, ‘wasted effort’, adjusting, needing to talk |
| Tully et al (2013), northeast England | Women, scheduled and unscheduled caesarean section, aged 18–41 years (n=115) | Understand women's perceptions regarding appropriateness of caesarean section births according to circumstances and views of choices | Semi-structured interviews conducted 1 day–a few days postpartum | Thematic content analysis | Rejected idea of ‘emergency’ vs ‘elective’ caesarean as over simplistic. Four main categories: unscheduled caesarean without medical indication, unscheduled caesarean for medical indication, scheduled caesarean without medical indication, scheduled caesarean for current medical indication. Women's preparedness for mode of birth and outcomes influenced feeling of agency over birth |
| Weckesser et al (2019), West Midlands, England | Primi- and multiparous women aged 26–45 years (mean 34.4 years), scheduled and unscheduled caesarean section (n=21) | Understand experiences of post-caesarean recovery and priorities for infection prevention | Semi-structured telephone interviews (n=6) and focus groups (n=15, 8 in group A, 7 in group B) conducted up to 6 months postpartum | Thematic analysis | Women lacked knowledge regarding post-caesarean complications and were unprepared for recovery period. Women's subjective experience of pain and ability post-caesarean influenced perception of how ‘successful’ their births were. Themes: experiences of pain, mobility, caregiving and everyday activities, infection experiences, knowledge and health seeking, infection information provision and needs |
| York et al (2005), northwest England | Women, unscheduled caesarean, aged 21–39 years (n=10) | Explore women's views and factors affecting decision to undergo a planned caesarean after a previous unplanned caesarean | Data collected during women's second pregnancy via semi-structured interviews; timeframe since previous birth not specified | Thematic analysis | Gaining control after previous unplanned caesarean is key indicator behind women's decision to undergo caesarean again. Women's decisions are made early on, with planned caesarean being perceived as the predictable option. Themes: women's concerns, mechanism of decision making, information |
Using the Critical Appraisal Skills Programme (CASP, 2020) checklist, the quality of the studies was shown to be high in regards to clarity of research aims, appropriate use of qualitative design, credible reporting of findings and implications for practice. Studies that emerged from larger quantitative surveys were more likely to score lower in regards to methodological quality indicators. The two unpublished studies were of high quality overall in comparison to some peer-reviewed studies, which could be explained by less restriction on word count, allowing for better reflexivity and in-depth description of the analytical process.
Thematic synthesis of the studies identified three key themes: ‘patient-clinician relationships’, ‘decision making as an emotional journey’ and ‘caesarean not really an informed choice’. Eight subthemes were derived from the overarching themes. Within the first theme, patient–clinician relationships, there were two subthemes: ‘women versus clinicians as decision makers’ and ‘clinician's role in facilitating agency’. Within the second, there were two subthemes: ‘“touchpoints” in decision making’ and ‘meaning of caesarean birth’. Within the third, there were four subthemes: ‘information seeking’, birth preparedness’, ‘recovery preparedness’ and ‘closure’.
Patient-clinician relationships
Women versus clinicians as decision makers
The phrase ‘jumping through hoops’ would best describe the experiences of women in the studies that chose caesarean section as their mode of birth (Mason, 2015). Women reported feeling infantilised and undermined as they circumnavigated maternity care structures that were perceived as unsupportive of their decisions because of ulterior motives or that did not offer comprehensive continuity of care systems, resulting in women continually feeling like they had to justify their decisions throughout (York et al, 2005; Mason, 2015; Kenyon et al, 2016). For some women, the wish to have a caesarean section stemmed from a sense of regaining control after a lack of perceived agency during previous childbirth. These narratives illustrated the power struggle and frustration of being dismissed by maternity care providers (Murphy et al, 2003; York et al, 2005; Fenwick et al, 2009; Tully and Ball, 2013; Kenyon et al, 2016). In contrast, women who underwent an unscheduled caesarean section reported having very little or no control over the decision. Women used threatening medical terminology to explain the urgency of the situation, and how there was no scope to make decisions during emergency circumstances (Murphy et al, 2003; Baston, 2006; Porter et al, 2007; Fenwick et al, 2009; Redshaw and Hockley, 2010; Tully and Ball, 2013).
‘We didn't have opportunity to discuss it [caesarean section] really. They said [the situation] was life or death and a threat to me as well.’ First time mother, 28 years
The theme ‘in safe hands’ in Baston (2006) illustrates how some women felt acceptance and even relief in handing over the reins to clinicians to make the decision for them. Contrastingly, ‘illusion of choice’ highlighted the concept of maternal choice as a tick-box exercise for clinicians (Murphy et al, 2003; Baston, 2006; Tully and Ball, 2013; Kenyon et al, 2016).
Clinicians role in facilitating agency
Clinician communication style was a key narrative in distinguishing perceptions of control and agency, particularly in unscheduled caesarean sections. Women's needs and preferences in regards to clinician care varied widely. For example, some women found confidence in their clinicians' speed and finality in performing surgery:
‘I don't think anybody introduced themselves to me… But that didn't bother me, ‘cos they just seemed to work really well as a team… and I just felt really happy that I was in good hands really’ 1375
Clinical staff banter and an informal approach were found to be reassuring and normalised a situation that was unexpected and frightening (Baston, 2006; Fenwick et al, 2009). However, for some women the rush, casualness or lack of communication only made women more anxious or served to de-humanise women who expressed feeling like ‘meat on slabs’ (Porter et al, 2007) or next in a ‘production line’ (Baston, 2006; Redshaw and Hockley, 2010). Overall, staff were described as ‘too busy’ or caught up in their workflow to offer more personalised care. Simple gestures, such as reassuring touches or having staff members talk through the process made women feel more involved in and satisfied with their caesarean section births (Baston, 2006; Porter et al, 2007; Fenwick et al, 2009; Redshaw and Hockley, 2010; Mason, 2015).
This theme demonstrates how care provider communication, both direct and indirect, can impact the relative power balance of women's decision-making process and overall experience of birth. This has implications for practice in terms of staff training needs (ie basic counselling skills) and in particular, how clinicians can best prepare women for medical situations where the notion of agency is subjugated by factors such as patient safety.
Decision making as an emotional journey
Touchpoints in decision making
Generally, women across the studies recognised vaginal delivery as the best option for themselves and their babies as deemed by society as what constitutes a ‘good mother’ (Mason, 2015). Therefore, the decision to undergo a caesarean section invoked many emotions including guilt, sadness, disappointment, self-blame, anger and relief (York et al, 2005; Baston, 2006; Fenwick et al, 2009; Redshaw and Hockley, 2010; Tully and Ball, 2013; Mason, 2015). Touchpoints or situations of emotive saliency in the decision-making process were named in three of the studies as important in women's subjective journey towards accepting or finalising the decision to give birth via caesarean section, and consequently how women remember their childbirth (Baston, 2006; Mason, 2015; Kenyon et al, 2016). For some women who had undergone unplanned caesarean section, these touchpoints were defining moments usually signalling a loss of control over childbirth (Baston, 2006; Redshaw and Hockley, 2010). For women facing the possibility of a caesarean section, the decision process was marred with anxiety related to the stigma of giving birth in this way. Women reported feeling relief once that decision was taken out of their hands, and felt like clinicians had a responsibility in aiding women to manage the emotional aspects (Baston, 2006; Tully and Ball, 2013; Mason, 2015). While others looked back at touchpoints with resentment, as this bookmarked how women failed to prevent an unwanted situation:
‘I believe if they had done scans they would have seen that the baby was big and breech and a C-section would have been planned’ 5051 UP
Meaning of caesarean birth
The subjective meaning women placed on caesarean section as a mode of birth related to women's acceptance and postnatal adjustment. Women's accounts can be categorised into two separate entities, the first is women who see mode of birth as a ‘gateway’ or meaningful transition into motherhood, in which caesarean section is seen as aberration to this process. On the other hand, some women perceive caesarean section as a means to an end, or a procedure that is necessary in order for them to receive their goal: a safe delivery and healthy baby (York et al, 2005; Baston, 2006; Fenwick et al, 2009; Mason, 2015).
‘It was just a really positive experience but to me the delivery was never important in a rite of passage sense’.
Sarah (Mason, 2015)
Women described assigning meaning to caesarean section births as a fluid process of internal negotiation. For example, some women thought of caesarean section as a sacrifice they have to go through for the sake of their baby (Baston, 2006; Tully and Ball, 2013). Additionally, some women reflected on how the final decision to undergo a caesarean section should have been facilitated earlier to allow reframing of birth expectations (Redshaw and Hockley, 2010; Mason, 2015; Kenyon et al, 2016). Themes like ‘just another new mother’ exemplify how a clinician's perception of caesarean section is more in line with the viewpoint of surgical birth as a routine medical procedure (Redshaw and Hockley, 2010).
Overall, this theme illuminates the incongruity between clinical decision-making models adapted by staff and the decision-making journey undertaken by women in reframing their childbirth ideologies. It can be observed that women's decisions or acceptance of caesarean section are shaped by larger constructs that go beyond institutional influence, such as societal pressures over what is defined as normative births.
Caesarean not really an informed choice
Information seeking
Women's accounts reflected information seeking as emotionally driven and multifactorial, where different information sources were consulted according to women's perception of needs. There was a sense from women's narratives that standardised, institution-level information did not cater to women's needs. Furthermore, women often felt the clinician's information was conflicting, biased or led by wider organisational priorities in promoting natural births (Murphy et al, 2003; York et al, 2005; Baston, 2006; Fenwick et al, 2009; Tully and Ball, 2013; Mason, 2015; Kenyon et al, 2016; van Griensven et al, 2016; Weckesser et al, 2019). Overall, women who underwent both scheduled and unscheduled caesarean section questioned if the timing, quantity, quality and format of formal information given truly enabled informed decision making (; York et al, 2005; Redshaw and Hockley, 2010; van Griensven et al, 2016).
‘My mum had a hysterectomy and the level of information she got for a fairly similar surgery was mountains and mountains. And we just like, don't have anything’ Focus Group A
Women highlighted the importance of lay information sources such as the media and other women's ‘birth stories’ in order to build their own narrative in regards to the meaning and realities of caesarean section (Mason, 2015). These women described cognitive bias in selecting information in order to preserve pre-existing beliefs or to validate their feelings.
‘My friends who have had emergencies and then electives, I wanted their opinion, just to reassure myself really’ Heather, bank clerk, 31 yrs
Birth preparedness
Overall, women's sense of preparedness in undergoing a caesarean section was linked to women's feelings of agency over their childbirth. Women who felt inadequately prepared for their caesarean reported more negative association surrounding the emotional and physical consequence. Words such as ‘shock’ were frequently used to illuminated how a caesarean section was not expected and in dissonance to what women were taught and encouraged to practice at antenatal classes (in their birth plan)(Murphy et al, 2003; Baston, 2006; Porter et al, 2007; Redshaw and Hockley, 2010; Weckesser et al, 2019). Lack of preparedness was also connoted with women feeling distress and fear during the surgery or associated operational procedures such as anaesthesia and even the operative room environment (Porter et al, 2007; Redshaw and Hockley, 2010; Mason, 2015; Tully and Ball, 2013).
‘The spinal injection and the sensation of hands working inside my body-I've always described it as “gutting a fish”’ 0319
For some women, this sense of detachment was transferred to their infants, with women reporting feeling ‘numb’ (Baston, 2006) and unable to bond immediately after birth (Baston, 2006; Porter et al, 2007; Fenwick et al, 2009).
‘I actually said “yes take him (baby) away”. Because I hadn't really felt as though I'd given birth or anything’ 305
Recovery preparedness
Both scheduled and unscheduled caesarean section first-time mothers reported a lack of knowledge regarding what to expect after caesarean section births, both in the short and longer term. Women's vulnerability and dependence on clinicians during the surgery was further compounded by women's feelings of helplessness afterwards (Baston, 2006; Porter et al, 2007; Fenwick et al, 2009; Mason, 2015; Tully and Ball, 2013; Weckesser et al, 2019). Some of the women reported their experience of having decisions made for them by a panel of experts during birth meant they were left with inadequate knowledge and tools to make postnatal decisions or having little awareness of how caesarean section could affect other maternal decisions such as breastfeeding (Baston, 2006; Redshaw and Hockley, 2010; Mason, 2015). Furthermore, women reported not factoring in the emotional and physical toll of balancing motherhood with postoperative recovery, and not being aware of the recovery duration as well as all the risks associated with caesarean surgery (York et al, 2005; Porter et al, 2007; van Griensven et al, 2016; Weckesser et al, 2019).
‘I don't feel as if anyone's ever informed fully of, one, how major an operation it is, and two, how long it's going to take to heal externally, but also internally, and the sort of pains and afterpains you get’.
32 (van Griensven et al, 2016)
Closure
Debrief was a key construct identified throughout the studies, as women mentioned a lack of opportunity to discuss and regain closure following their caesarean section births. Women explained debrief as more involved than giving out postnatal recovery information (Murphy et al, 2003; Baston, 2006; Mason, 2015; Redshaw and Hockley, 2010; Fenwick et al, 2009).
‘I can't remember anyone actually talking to me about post-caesarean, and how I might feel about it. I think it was all at the physical end, not at the mental end’.
1343 (Baston, 2006)
Women highlighted the important yet unfulfilled need for debriefing to make sense of or normalise their experience. Clinicians' lack of acknowledgement over how women were left feeling about their births served to reinforce feelings of lack of ownership over the birth.
‘But that got me nowhere (crying). That didn't get anybody to say “Oh, I'm really sorry about that” or “why do you feel angry”. It didn't even get anybody to say, “explain to me why you feel like this”’.
1375 (Baston, 2006)
This theme encapsulates women's unmet needs in regards to practical information and emotional support. Misalignment between caregivers perception of caesarean section as a routine event where clinical input ceases when the goal of successful delivery is achieved, versus caesarean section as an important beginning to motherhood is again illustrated by the postsurgical care precipice and a lack of opportunity for debriefing.
Discussion
This review synthesised qualitative findings from 11 studies, with interlinked themes, and highlighted patient-clinician dynamics as a key factor underlying how women feel about their birthing decisions. Accounts echo previous findings that mode of birth does not solely influence maternal satisfaction or outcomes (Spaich, 2013; Bell and Andersson, 2016). The complex interplay of intrapartum experiences can better explain women's processing of caesarean section births. These experiences include institution-led care pathways and inaccessibility of equitable information, leading to discrepancy in expectations.
Current UK guidelines promote the golden standard of caesarean section as maternal choice, as long as the woman is adequately informed and accurately aware of the risks and benefits, and the role of the clinician is placed as expediter of this process (NICE, 2013). Findings from this review indicate that there is minimal evidence of caesarean section births, either scheduled or unscheduled, being the product of a shared decision-making process. The theme ‘patient-clinician relationships’ illustrates the imbalance of influence between women and clinicians that was found in the reviewed studies. The findings indicate that women's involvement preferences vary widely; these variations in findings can perhaps be explained by the difference between the ‘what’ and ‘how’ in provider communication (Patterson et al, 2019). Women who experienced empathic, personalised care from their providers were more likely to perceive their experience favourably, even in scenarios where women had low levels of control over what was happening to them.
A lack of preparation was identified as a prominent narrative and key indicator that women do not undergo caesarean section as an informed procedure. Women who underwent unscheduled caesarean sections reported that they were not expecting to give birth surgically and did not fully understand the reasons or implications surrounding their childbirth. Even women who expected their caesarean section births reported not fully anticipating the postsurgical physical and psychological debilities. Moreover, women were not fully aware of the risks or potential complications of surgical birth, further putting into question ethical issues surrounding consent and informed choice. For some women, the dissociation experienced in the theatre carried over to parturition, with women reporting numbness or loss of attachment to their babies. These findings are comparable with what is already seen in the literature, which includes post-caesarean section emotional difficulties ranging from mood disturbances to PTSD. These are more marked in women who experience unscheduled caesarean section. Furthermore, this detachment can be explained by the interlinked triad of loss of control over birth decisions, mismatch in expectations of a momentous occasion and poor woman–provider interrelationships (Lobel and DeLuca, 2007; Puia, 2013; Kjerulff and Brubaker, 2017; Benton et al, 2019).
Findings from this review have important implications for practice in that provider discourse and standard antenatal education packages with a heavy focus on natural births as the norm are not discouraging surgical births, but are impacting on how women feel about their decision or their experience of caesarean section births. With one in four women giving birth via caesarean section currently in the UK (Paranjothy, 2004), there is a responsibility to include caesarean section births as part of routine conversation in obstetric care and the antenatal curriculum offered to expecting women and families. In this regard, increasing the quantity and quality of impartial information regarding all birth modes will not only aid shared decision making, but also promote acceptance for those that had not planned their caesarean section.
Limitations and recommendations
There are a number of caveats to this systematic review. First, almost half of the studies included (n=5) were published more than 10 years ago (Murphy et al, 2003; York et al, 2005; Baston, 2006; Porter et al, 2007; Fenwick et al, 2009). Current research is needed in order to extrapolate how (or if) changes in care practice (ie skin-to-skin initiatives) have impacted on women's feeling of agency in the decision-making process and general caesarean section birth experiences.
Second, a disproportionate number of women who participated in the studies were of white British ethnicity, employed and in a relationship at the time of birth. Evidence indicates that immigrant women and women of black ethnicities are more likely to experience birth complications resulting in surgical intervention (Royal College of Obstetricians and Gynaecologists, 2001). Moreover, there is evidence that women's faith-related needs are not well understood by care providers (Firdous, 2020). Further research is necessary to explore the decision-making experiences of black and minority ethnic women, who are statistically more likely to go through unscheduled caesarean section births (Royal College of Obstetricians and Gynaecologists, 2001), and likely to have additional needs because of cultural and language barriers. The findings from this review illustrate that women are not passive receivers of information, rather decision making or decision reviewing consists of complex mental heuristics that are often situational. It remains unclear how medically trained clinicians working within limited capacity can best support women that are more vulnerable, despite the increase in prevalence of women with additional needs, such as refugee women, accessing NHS maternity services (Higginbottom et al, 2019).
The quality appraisal of the reviewed studies indicated methodological flaws, which can be addressed in future studies. Of note, most studies did not explain the authors' process or rationale in purposively sampling participants that originated from larger quantitative studies, putting into question the breadth of the accounts and qualitative research rigour (Meyrick, 2006). Overall, high-quality qualitative and quantitative research with a focus on improving the diversity of accounts are needed to gain a better understanding of patient experiences for service improvement.
Conclusions
Women assign meaning to birth mode, with some women rejecting the concept of surgical births more than others do. The promise of choice and informed decision making in obstetrics can be misleading, as this connotes an element of control over a natural or surgical situation that can be unpredictable and often uncontainable. It is clear from women's accounts that maternity care providers have a role in preparing women for the realities of birth and facilitating agency in situations that are outside women's control. As the number of caesarean section births is predicted to increase (Betrán et al, 2016), it is important that women's decision-making requirements are met in order to foster healthier mother-infant outcomes.
Practice recommendations
Based on these findings, the authors recommend standardisation of maternity care policy and practice that endorses shared decision making, including clinician skills training or upskilling in emotional aspects of birth A shift towards antenatal education programmes that destigmatises caesarean section as a common birth procedure and de-mystifies birth aspects in general would also be beneficial, as well as the availability of timely ante- and postnatal information that is objective and accessible. This includes giving post-caesarean women opportunities to debrief in a way that is mindful and empowering.
Key points
- National guidance stipulate informed consent as key to better birth outcomes; however, there is a lack of understanding regarding women's decision-making experiences in regards to caesarean births
- This systematic review uncovered three interconnecting themes: patient–clinician relationships, decision making as an emotional journey, and caesarean not really an informed choice
- These themes illustrate how complex factors such as clinician communication can influence women's sense of agency over their caesarean births, and their satisfaction with this outcome
- Findings suggest tailored care pathways with a focus on continuity of open dialogue regarding birth options (including postnatal debrief) endorse shared decision making in childbirth


