Caesarean section rates have steadily increased, with global rates of 21.1% almost doubling since 2000 (Zewude et al, 2022). World Health Organization (WHO, 2021) records show that caesarean section rates grew from 7% in 1990 to 21% in 2021. By 2030, it is predicted that one-third of all births will likely be by caesarean section (WHO, 2021). This escalation is associated with an increase specifically in women choosing to have a caesarean section, as over 40% of caesarean sections are elective (Evans et al, 2022). This indicates a need to understand the driving factors and perceived benefits behind decision making in relation to mode of birth (Miller et al, 2016). It has been suggested that caesarean section may be seen as an easier option, although there is limited evidence to support this (Loke et al, 2015). Tuschy et al (2018) suggested that it was the result of advancements in medical procedures and equipment, as well as guidelines supporting women's autonomy in decision making (National Institute for Health and Care Excellence, 2019).
In health policy, there has been a shift towards patient autonomy in care planning (Fawsitt et al, 2017) that seemingly encourages elective caesarean section, despite guidelines advocating its use only for medical reasons (WHO, 2015; National Institute for Health and Care Excellence, 2019). Satisfaction with childbirth is also closely related to a woman's involvement in decision making on mode of birth and outcomes (Buyukbayrak et al, 2010). In the literature, the reasons behind women's choice of mode of birth and common postpartum outcomes have been considered separately, but few studies map choice of method to quality of life after birth. It is important that obstetric care incorporates the latest evidence in order to provide women with up-to-date knowledge about different modes of birth, especially in the digital era when women can seek alternative information sources.
In many countries, including the UK, the postpartum period spans from childbirth to 6 weeks after birth, when the uterus has regained its original size (Borders, 2006). However, this can lead to, physical, mental and social postnatal outcomes that fall outside this timeframe being disregarded, as they take place after scheduled postnatal checks are completed (Triviño-Juárez et al, 2017; NHS, 2022). This review's aim was to explore decision-making factors and postnatal quality of life, comparing caesarean section and vaginal birth. The objectives were to identify factors that influence choice of mode of birth, to investigate the short- and long-term postnatal outcomes unique to caesarean section and vaginal birth, and to identify areas for monitoring and support after birth.
Methods
This narrative literature review focused on comparing caesarean section with vaginal birth in relation to decision making and postnatal outcomes and quality of life. A narrative review was deemed the most appropriate approach as the aim was not just to summarise existing data, but to identify major themes, reveal gaps in research and suggest new ideas, which this review type is particularly useful for.
Eligibility criteria
Inclusion and exclusion criteria were established using the PICOS framework (Huang et al, 2006; Brown, 2019): as follows:
- Population: women who gave birth through caesarean section, emergency caesarean section, vaginal birth or assisted vaginal birth
- Intervention: caesarean section, emergency caesarean section, vaginal birth or assisted vaginal birth.
- Comparison: decision-making factors for the interventions and their associated postnatal outcomes
- Outcomes: postnatal quality of life.
- Study design: qualitative, quantitative or mixed methods studies that met appraisal requirements.
This framework provided the elements to create the research question, which was ‘what are the factors affecting women's decision making on mode of childbirth and the postnatal outcomes of caesarean section compared to vaginal birth?’.
Search strategy
Electronic databases (Google Scholar, PubMed, Medline and Wiley Online Library) were searched between February and June 2023. Keywords extracted from the research question were combined for the search: caesarean section, vaginal birth, decision making and postpartum outcomes. From these, other search combinations were created where a term could be truncated to account for variations and increase search sensitivity. Boolean operators ‘OR’ and ‘AND’ facilitated extensive inclusion of relevant research. Alongside the studies from the search, reference lists, similar articles and ‘cited by’ columns were also assessed for widespread data discovery. To capture the latest, evidence-based information on this topic, studies dated before 2000 were excluded, as were studies that did not meet the Critical Appraisal Skills Programme Tool (2023) appraisal checklist requirements, such as a relevant methodology, rigorous data analysis and a clear documentation of the findings. Studies not written in English were also excluded to avoid possible errors from misinterpretation of language, which can negatively affect the credibility of research results.
Screening
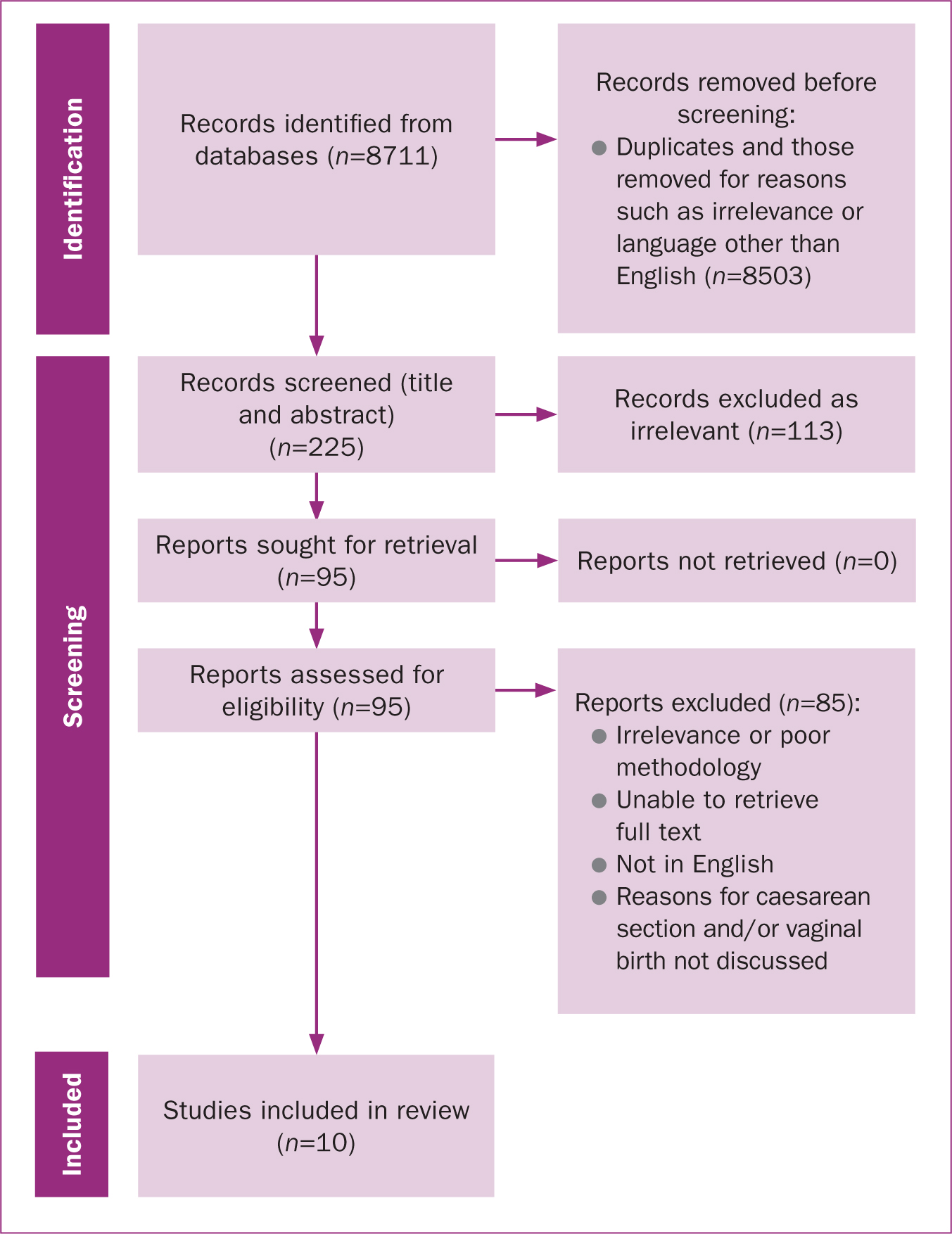
In total, 8711 articles were initially identified, with 8503 duplicates and irrelevant articles removed, leaving 208 articles. After assessing titles and abstracts, full texts were retrieved and assessed for eligibility (Page et al, 2021; Critical Appraisal Skills Programme, 2023). Of the 208 articles, 113 were excluded. Recurrent reasons for exclusion were inapplicable methodology and a lack of evidence-based information about factors that lead to decision making on childbirth and/or the postpartum outcomes. A total of 10 articles were included after mapping their content with the aims outlined for this study (Figure 1).
Analysis
Thematic analysis was done in line with Braun and Clarke's (2006) steps. First, keywords from the research question were identified, including caeserean section, vaginal birth, decision making and postnatal outcomes. Next, papers were assessed repeatedly and thoroughly, prioritising keywords and recurrent themes were identified. Finally, the themes were developed, where similar concepts were brought together, compared and discussed.
Results
This review included 10 studies with a combined sample of over 180 000 women from a number of countries around the world. The studies' key characteristics are summarised in Table 1.
| Reference | Location | Number of participants | Methods |
|---|---|---|---|
| Borders (2006) | USA | Not stated | Literature review |
| Buyukbayrak et al (2010) | Istanbul, Turkey | 1588 | Qualitative cohort study |
| Cook and Loomis (2012) | Ontario, Canada | 15 | Qualitative, phenmenological study |
| Loke et al (2015) | Hong Kong | 319 | Descriptive cross-sectional study |
| Bossano et al (2017) | USA | 576 | Supplementary longitudinal cohort study |
| Petrou et al (2017) | England | 2161 | Prospective population-based study |
| Fobelets et al (2018) | Germany, Ireland and Italy | 1831 | Prospective longitudinal survey |
| Akgün and Boz (2019) | Antalya, Turkey | 12 | Phenomenological qualitative study |
| Coates et al (2020) | Australia | 156 666 | Systematic scoping review |
| Evans et al (2022) | England, Ireland, Italy, Iran, Germany and Spain | 19 879 | Systematic review and meta-analysis |
After analysis, three themes emerged: intrinsic decision-making factors, extrinsic decision-making factors and the association between mode of birth and physical and mental postnatal outcomes.
Intrinsic decision-making factors
Intrinsic decision-making factors in relation to mode of birth emanated from women's unique experiences and beliefs (Buyukbayrak et al, 2010). These included sociodemographic factors such as age, parity, socioeconomic status and education, and those based on women's views (Bossano et al, 2017; Coates et al, 2020).
The selected studies highlighted that many women preferred a vaginal birth (Buyukbayrak et al, 2010; Cook and Loomis, 2012; Loke et al, 2015; Akgün and Boz, 2019; Coates et al, 2020). Some believed that vaginal birth was the ‘natural’ method for birth or chose to have a vaginal birth after a previous caesarean section for emotional satisfaction (Akgün and Boz, 2019). In some countries, such as Nigeria, religious beliefs led women to reject a life-saving caesarean section (Coates et al, 2020). However, where their beliefs did not discourage it, a preference for caesarean section was associated with previous experience of caesarean section and increased parity compared to first-time mothers (Coates et al, 2020). Akgün and Boz (2019) and Coates et al (2020) noted that past childbearing experiences strongly influenced mode of birth in future pregnancies, as a disappointing experience with vaginal birth could discredit this method for parous women. However, these studies did not separate women who had a caesarean section for medical reasons from those who had an elective caesarean.
Some studies reported that financial affluence made elective caesarean section more desirable, as it allowed scheduling of the birth and there was a misconception that it was easier than vaginal birth (Coates et al, 2020). Caesarean section was seen as a fashionable mode of birth across social groups in high-income countries, such as Australia (Coates et al, 2020). Loke et al (2015) reported that choosing to have a caesarean section was linked with lower health education levels.
Fear of labour pains motivated women who chose an elective caesarean section, while fear of surgical interventions motivated women who chose to have a vaginal birth (Borders, 2006; Loke et al, 2015; Coates et al, 2020).
Extrinsic decision-making factors
External influences significantly impacted women's choice of mode of birth. These influences included healthcare professionals, relatives and cultural norms. While some studies reported that doctors and midwives had a strong influence on a woman's choice (Buyukbayrak et al, 2010; Cook and Loomis, 2012), others highlighted that women's decisions were directly linked to information that they received from their friends and relatives (Loke et al, 2015).
Cultural norms that were prevalent not just in the society that women found themselves but also among healthcare professionals providing care to women also impacted decision making. In areas such as Turkey, more doctors advocated for repeat caesarean section without medical indication (Akgün and Boz, 2019), while in the UK doctors generally encouraged vaginal birth even after a previous caesarean section (Cook and Loomis, 2012). The experiences of and advice from a woman's close relatives also motivated and informed her choices (Coates et al, 2020). Social norms impacted mode of birth by informing the practices of healthcare professionals and the choices of women (Coates et al, 2020).
Physical and mental postnatal outcomes
The studies considered postpartum quality of life between time periods spanning 1 hour (immediate) to 15 years (long term) after birth. In the immediate postpartum period, up to 94% of women experienced at least one health problem including pain, bleeding or incontinence, regardless of mode of birth (Borders, 2006). Similarly, factors such as advanced age, existing illnesses and prolonged recovery time reduced quality of life for women who had both caesarean sections or vaginal births (Fobelets et al, 2018).
Subjectively, quality of life was improved for women who had a spontaneous vaginal birth compared to those who had an assisted vaginal birth or elective or emergency caesarean section, and these results remained consistent long term for both physical and mental health (Petrou et al, 2017; Fobelets et al, 2018; Evans et al, 2022). Emergency caesarean section and assisted vaginal birth ranked lowest in quality of life domains across several studies (Borders, 2006; Bossano et al, 2017; Fobelets et al, 2018). Despite findings in older studies that mode of birth has no association with postpartum depression (Fobelets et al, 2018), Evans et al (2022) reported that up to 30% of mothers experienced postpartum depression in the first year, especially if their expectations did not match the outcomes. All of the reviewed studies highlighted issues relating to under-reporting of postpartum health problems by mothers.
Discussion
This literature review was conducted to explore the factors that influence decision making regarding mode of birth, and how postnatal quality of life is impacted by the choice women make. There are concerns relating to the increasing morbidity associated with elective caesarean sections, which form a significant proportion of all caesarean sections (Evans et al, 2022). This highlights the importance of understanding how women make decisions in relation to mode of birth, and how those decisions can affect the lives of themselves and their babies.
Decision making
Both intrinsic and extrinsic factors contributed to women's decision on mode of birth. Physical and mental postnatal outcomes could be affected by their choice. Women's decisions could be influenced by culture and socioeconomic status. Although this cannot be generalised to entire populations, predominant cultural norms in a region are known to strongly influence childbirth (Ryding et al, 2016). Financial affluence also affects how women view childbirth (Buyukbayrak et al, 2010); an elective caesarean section costs more than a spontaneous vaginal birth (NHS, 2021), meaning that more affluent women may prefer a caesarean section and link it with perceptions of ease and prestige (Coates et al, 2020). However, women in countries without universal care may choose a vaginal birth as a cost-effective option (Chabbert et al, 2021).
Coates et al (2020) suggested that the aforementioned factors were outweighed by healthcare professionals' influence on women's choice. For example, in Spain, only 15% of obstetricians are reportedly willing to perform an elective caesarean section, compared to 79% in the UK (Wise, 2018). The influence of external factors on mode of birth decision making mean that it is crucial that the best evidence is widely circulated to debunk myths, maintain safe caesarean section rates and ensure perinatal safety for mother and child.
Quality of life
Postpartum quality of life was measured using generic tools, such as the Salmon questionnaire (Bossano et al, 2017) and short-form-six-dimension tool (Fobelets et al, 2018), which assesses fulfillment. Mokhtaryan-Gilani et al (2022) criticised these tools, on the basis that they lack participant-specific context. However, Fobelets et al (2018) defended them as reflecting the population's preferences in maternity care settings. There are numerous ways to collect qualitative data, each deemed most appropriate by the researcher. No one tool encapsulates all the qualities needed to capture participants' thoughts; however, any tool used should customise value sets that consider the economic and cultural peculiarities of the population involved, offering open-ended questions that participants can explore subjectively.
The reviewed studies found improved quality of life for women who had vaginal births, compared to those who had caesarean sections, in terms of both physical and mental domains, such as pain and depression (Bossano et al, 2017; Petrou et al, 2017; Fobelets et al, 2018; Evans et al, 2022). However, other studies have reported no differences in quality of life, regardless of parity or in cases of multiple pregnancies, and found no differences in outcomes between vaginal birth and caesarean section in women with more than one child (Hutton et al, 2015; Triviño-Juárez et al, 2017; Rezaei et al, 2018). These differences may be the result of different study methodologies, tools used to assess quality of life and study locations. For example, the Short Form Health Survey and Salmon Questionnaire tools, which were used in the selected studies to assess quality of life, were based on preset questions. This standardised method is arguably not a thorough approach to collecting data about choices and experiences, which are subjective. Furthermore literacy levels and time factors could affect communication from participants (Stefanacci, 2024). Healthcare professionals need to keep in mind that assessing quality of life requires thoughtful communication and active listening, making every contact count and offering appropriate referrals for further support where needed.
Postpartum life continues for years after childbirth and encompasses the physical, mental, social and financial realities of parenthood (Petrou et al, 2017). Although Borders (2006) reported that almost all women experienced at least one postpartum health problem shortly after birth, regardless of mode of birth, Bossano et al (2017) highlighted that vaginal birth yielded better outcomes in the longer term, looking for up to 10 years after birth. It is important that these results are viewed as tendencies and not absolutes when caring for individuals, as they are subject to change with emerging trends in obstetric care and with unique experiences of pregnancy.
Education and financial status were both linked to postnatal outcomes, with women who had attended higher education and those with greater socioeconomic status having better postnatal outcomes whether they gave birth by caesarean section or vaginal birth (Bossano et al, 2017; Fobelets et al, 2018). These findings highlight the importance of taking non-medical health determinants into account when assessing postnatal outcomes. Borders (2006) highlighted that women with existing problems, such as stress and social exclusion, experienced postpartum morbidities that were often underestimated. Similarly, Petrou et al (2017) reported speedier postpartum recovery for mothers with access to social support and fewer financial difficulties.
Fear of pain as a decision-making factor for caesarean section implied the perception of greater pain in vaginal birth; however, caesarean section is associated with increased physical morbidity and poorer quality of life postnatally (Petrou et al, 2017). Conversely, vaginal birth did not always produce better outcomes. Studies showed that women who had an assisted vaginal birth fared worse postnatally than all other birth methods (Borders, 2006).
The reviewed studies restricted assessment of postpartum quality of life to physical and mental elements of health, ignoring social, financial and psychological domains, although these were part of the decision-making process for pregnant women (Bossano et al, 2017; Akgün and Boz, 2019). This is partly because the assessment tools did not include psychosocial and economic components. The WHO (2015) recognises that psychosocial health determinants greatly impact health and wellbeing. Giving birth to a child can significantly alter socioeconomic status, and poor childbirth outcomes are likely to impact a family's financial status (Kim et al, 2018). Women with a low socioeconomic status are more likely to have caesarean sections because they are less likely to attend perinatal education, which is associated with opting for a caesarean section (Kim et al, 2018; Milcent and Zbiri, 2018).
The physical and mental domains of postpartum quality of life are interrelated. For example, physical morbidity can impair a woman's ability to breastfeed, leading to psychological distress (Bossano et al, 2017). Where there is psychological distress, physical health is worsened (Petrou et al, 2017). Surgical interventions associated with caesarean sections and assisted vaginal birth mean longer physical and psychological recovery times with delayed mother-baby interactions compared to vaginal birth (Karlström et al, 2011). This may partly explain the resulting decline in postpartum quality of life among women who have had a caesarean section.
Implications for practice
Health policies should explore the use of decision-making aids that outline the evidence of the risks, benefits and outcomes associated with different modes of birth. This will empower women in making informed choices. Although circumstances can change, this is a flexible way of putting mothers at the centre of the care (Bossano et al, 2017). As the long-lasting stretch of the postnatal period has been established as surpassing the first 6 weeks after childbirth, so should postnatal services aimed at mothers. Regardless of when a problem stemming from childbirth is noticed, women should be confident that on speaking to a healthcare professional, they will be listened to compassionately and signposted to adequate help. They can then go on to fully recover postnatally, function well in their new role and promote the development of their newborns.
Limitations
Although, this study encompassed a wide variety of participants from different countries, it lacks specificity; the results cannot be said to mirror the expectations and experiences of any one location or group of women. Thus, the results should be carefully applied to specific groups in consideration of their unique qualities and needs.
Conclusions
In order to support informed decision making in relation to pregnancy and birth, women need evidence-based information on modes of birth and their related outcomes. Women's choices are influenced by their environment and relationships. Informed choice and consent are only possible when women are educated on the different modes of birth and the short- and long-term outcomes. This practice also addresses concerns about the increasing morbidity associated with elective caesarean sections. Shared decision-making in childbirth between the woman and healthcare professionals involved in her care combines the clinicians' expertise with a woman's expectations and experiences. To adjust to changing trends in childbirth, obstetric support should target unhealthy cultural norms, aiming to end unhealthy practices by providing evidence-based education on modes of birth and their outcomes from early in pregnancy.
Key points
- Intrinsic and extrinsic factors can influence a woman's decision making on mode of birth.
- These factors can include perceptions of fear or safety, age and parity, previous birth experiences, personal values, socioeconomic status and education.
- In high-income countries, elective caesarean section rates are much higher.
- All reviewed studies highlighted under-reporting of postpartum health problems in mothers.
- Women need exposure to evidence-based information regarding mode of birth and related outcomes.
CPD reflective questions
- What information can you provide in your practice around mode of birth and related outcomes?
- Could shared decision making for mode of birth be improved in your practice?
- Do you feel that postnatal support is always signposted to new parents in your area of practice?
- What postnatal support could you signpost to?


