Increasing numbers of women, either during the birth process or in the postnatal period, require an indwelling urinary catheter for a number of reasons. This could be because the woman requires a caesarean section, or because she has been given epidural anaesthesia as a form of pain relief during labour and is therefore unable to pass urine. Alternatively, she may have had a postpartum haemorrhage and insertion of a catheter is recommended (National Institute for Health and Care Excellence (NICE), 2014a).
There are two types of catheterisation: intermittent, where the catheter is inserted into the bladder through the urethra and removed as soon as the bladder is drained of urine; or indwelling, where the catheter is inserted into the bladder through the urethra and left in place to continuously drain the bladder. Whatever the reason or method, where possible it is essential that the procedure and complications of catheterisation are discussed fully with the woman.
Urinary catheterisation is a common preoperative procedure undertaken prior to an elective or emergency caesarean section. In a survey of UK obstetricians, 82% reported using an indwelling catheter for both the procedure and postoperative management (Wee et al, 2005). The reasons for catheterisation prior to a caesarean section are fourfold:
However, there is insufficient evidence to support the routine use of catheterisation prior to a caesarean section (Abdel-Aleem et al, 2014).
Research has shown that it can take up to 8 hours for bladder sensation to return to normal after the last epidural top-up (Khullar and Cardozo, 1993). During this time, more than 1 litre of urine may be produced and, because the normal female bladder capacity is approximately 500 ml, the production of excessive urine may result in gross over-distension of the bladder.
Because a woman's bladder is particularly susceptible to myogenic injury secondary to over-distension, she may fail to void effectively—if at all—ever again. Hinman (1976) argued that a single episode of over-distension of the bladder can produce chronic changes in urethro–vesical function due to irreversible damage to the detrusor. However, some commentators suggest that (Walsh, 2007: 8):
‘The faulty thinking of basing a universal policy on a one-off, worst case outcome (bladder damage resulting in one missed case of bladder distension) may be driving intervention in this area.’
This is supported by De Sevo and Semeraro (2010: 11), who proposed that the psychological effects of catheterisation on healthy labouring women is potentially damaging:
‘When women are catheterized [during labour], they're given the message that “you can't urinate by yourself”—despite the fact that this is a bodily function they've been performing independently since they were toddlers.’
Women should be provided with every opportunity and support to pass urine normally prior to catheterisation. This includes privacy and, if possible, the opportunity to use a toilet. For women who are unable to use a toilet due to an epidural, the head of the bed should be raised to support the woman's back and she should be assisted to sit in the correct anatomical position.
‘Although catheterisation is rarely contraindicated, wherever possible the procedure should be avoided due to a range of potential complications’
Indications for catheterisation
Some women will require catheterisation for various reasons (Table 1). Although catheterisation is rarely contraindicated, wherever possible the procedure should be avoided due to a range of potential complications (Table 2). As previously highlighted, it is clearly preferable to avoid catheterisation, and women should be encouraged to use a bed pan at regular intervals during labour and the immediate postpartum period.
| Inability to pass urine during the antenatal period due to retroverted uterus |
| Prior to caesarean section |
| During labour if unable to micturate |
| Bladder filling for a prolapsed umbilical cord |
| During the third stage of labour, as a full bladder will prevent the uterus contracting |
| Women who are critically ill e.g. following major obstetric haemorrhage, pre-eclampsia |
| Retention of urine at any stage |
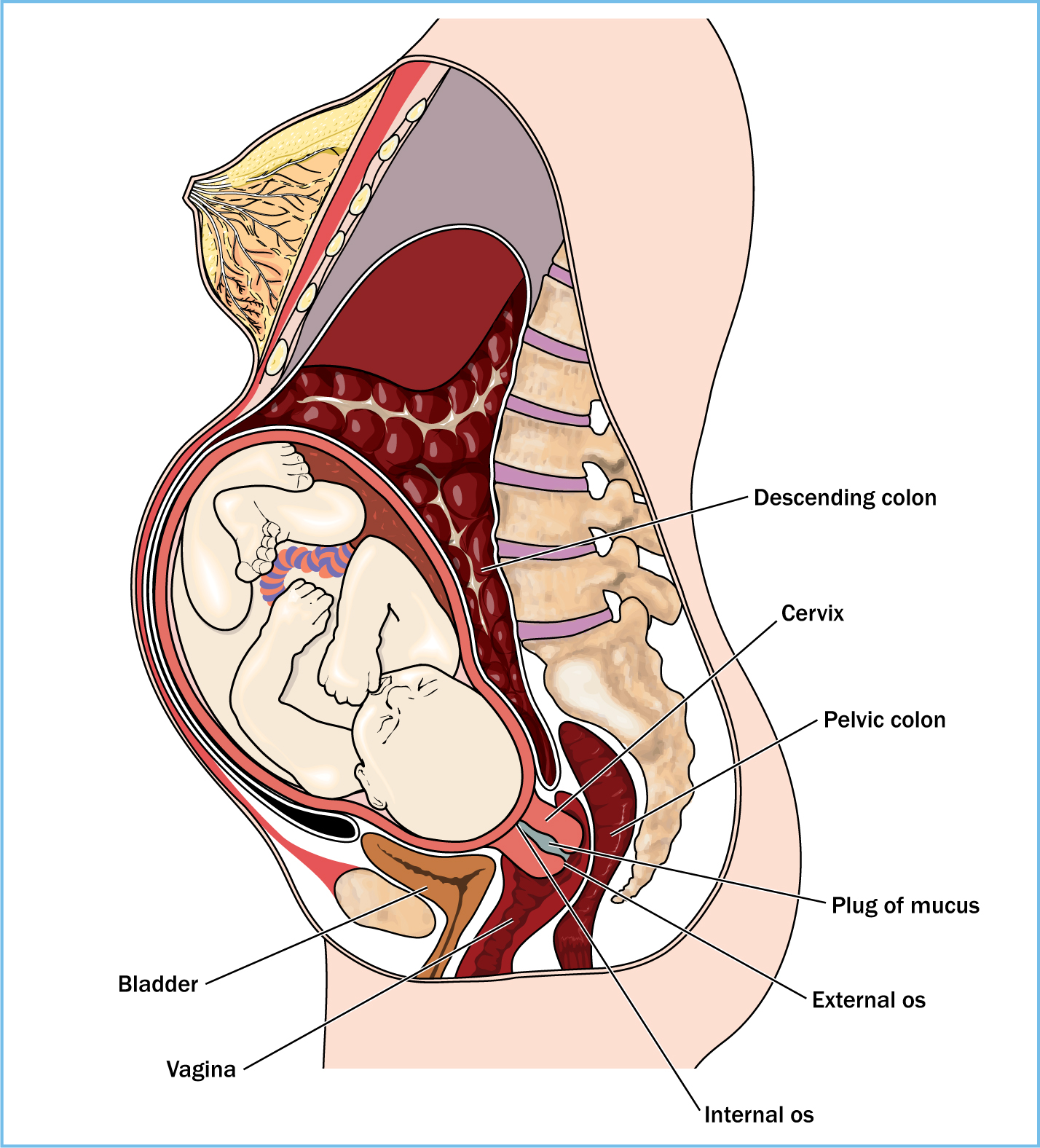
It is crucial that all midwives have a full understanding of the anatomy and physiology of the bladder, remembering that the bladder is a hollow muscular organ situated in the anterior part of the pelvis, below and in front of the uterus when empty (Figure 1). When the bladder is full of urine it extends upwards beyond the brim of the pelvis, and can be palpated above the symphysis pubis. A full bladder can displace the uterus and may lead to a prolonged labour and prevent involution of the uterus in the postpartum period.
The female urethra is approximately 4 cm long and, as such, it is easy to introduce infection if sterile techniques are not observed. Traditionally, in obstetrics, this procedure is undertaken without the use of local anaesthetic gel or any lubricant. The female urethra is lined with urothelium, lies flat like a ribbon in unequal and changing folds, and because it does not have any lubricating glands it is easily damaged and at greater risk of trauma. Such damage or trauma may be exacerbated during labour, especially if the baby's head is low, because the midwife or doctor will have to change the angle of the catheter slightly to pass over the head, thus increasing the potential for the trauma to the urethra.
Intermittent catheterisation
Intermittent catheterisation is where a catheter is introduced to drain the bladder, then removed. These catheters are generally made from PVC and have a hole at the tip of the catheter. A systematic review on short-term bladder drainage in adults stated that the use of intermittent catheterisation reduces the chances of infection (Niël-Weise and van den Broek, 2005).
Indwelling catheterisation
Indwelling catheters are made to be left in place and are often referred to as Foley catheters. These catheters have a balloon on the lumen of the catheter (Figure 2), which is inflated by 10 ml water (check manufacturer's recommendations); this ensures that the catheter is retained in the bladder. A catheter bag is then attached to the urinary catheter, thus ensuring a closed system. The majority of Foley catheters are made of latex and, as such, the midwife will need to establish any allergies prior to the procedure and be aware that latex can cause irritation in women who have epidural anaesthesia—this may not always be immediately apparent.

Catheter size
Catheters are sized according to the Charriere scale, which grades the outer circumference of the catheter (Nazarko, 2010). The smallest possible catheter should be selected to ensure a free flow of urine—this is usually size 10 Ch. Larger sizes can cause trauma and leakage of urine.
Procedure for catheterisation
First, assess the need for the procedure. This could be established by talking to the woman, taking a history and establishing her fluid intake, and undertaking an abdominal palpation.
‘It is necessary to gain informed consent and inform the woman of the possible complications of catheterisation’
If the procedure is indicated (Table 1), it is necessary to gain informed consent from the woman and inform her of the possible complications of catheterisation. If the woman is unable to speak English, an interpreter should be used. Ensure privacy at all times, and gather all equipment prior to the procedure. All hospitals have local guidelines on this procedure. It is now recognised that an appropriate anaesthetic, antiseptic, lubricating gel can help reduce infection, trauma to the urethra and pain—it is strongly advisable that this is used in all cases of catheterisation.
Potential complications
Pain
Pain can be caused by the introduction of a catheter into the urethra. As previously discussed, the lining of the uretha has no natural lubrication and is very sensitive. Pain may also be the result of trauma to the tissue or infection, which may be introduced during the procedure.
Tissue damage
Tissue damage can be minimised by using a lubricating gel, using the correct size of catheter and gently inserting the catheter, especially when the head of the baby is low. Repeated attempts at insertion of the catheter should be avoided.
Infection
The main risk factor for catheter-associated urinary tract infection (UTI) is duration of catheterisation (Loveday et al, 2014; NICE, 2014b; Velinor, 2015). Microorganisms causing catheter-associated UTI may gain access to the urinary tract either extra-luminally (as the catheter is inserted, by contamination of the catheter from health professionals' hands, perineal flora or microorganisms ascending from the perineum) or intra-luminally (by reflux of microorganisms from a contaminated urine drainage bag) (Velinor, 2015).
Contaminants that can be introduced include both bacteria and yeasts, such as:
The introduction of infection can be minimised by using a strict aseptic technique together with the use of an antiseptic gel. If the catheter is misplaced into the vagina this must be discarded and a new catheter used.
The signs of a UTI include:
Bladder damage
Damage may occur with long-term use of a catheter, and may also occur in women that need longer-term indwelling catheters. Nazarko (2007) suggests that, in such cases, the use of catheters with valves, which allow the bladder to fill normally and be drained when full, should be considered.
Conclusion
Pomfret (2007) suggested that all health professionals involved with urinary catheterisation should follow evidence-based guidelines to reduce the risk of complications (Table 3). However, the best advice is, wherever possible, to avoid the procedure during pregnancy and the postpartum period.
| Catheterise only when necessary—full assessment prior to procedure will determine clinical need |
| Obtain informed consent |
| Consider the use of intermittent catheterisation |
| Remove catheter as soon as possible |
| Monitor drainage—position drainage bag below the bladder and off the floor |
| Use the smallest size catheter gauge |
| Use analgesia and a lubricant from a single-use container prior to catheterisation |
Key Points
Revalidation claim: Continuing professional development/40 hours
This section provides an example of how this article might be used as material for reflection for use as part of a midwife's revalidation with the Nursing and Midwifery Council (NMC). Evidence for revalidation should be linked to the NMC Code and should demonstrate the impact that the learning has had on your practice.
Step 1: Context for the revalidation claim (link your learning activity to the Nursing and Midwifery Council Code)
| Nursing and Midwifery Council Code | Description | Focus of revalidation claim √ |
|---|---|---|
| Prioritise people | Act in the best interest of people (service users) at all times | √ |
| Practise effectively | Use best available evidence to assess client need and deliver treatment/care/advise on care | √ |
| Preserve safety | Work within your skills and knowledge (competence) and use your skills and knowledge to keep people (clients) safe | √ |
| Promote professionalism and trust | Act in line with the standards of practice and behaviour to uphold the reputation of the nursing and midwifery professions | √ |
Nursing and Midwifery Council (2015) The Code: Professional standards of practice and behaviour for nurses and midwives. NMC, London
Step 2: Contextualising your learning
| What did you think about on reading this clinical practice article? | This article was a good reminder for the indications of bladder catheterisation during pregnancy, labour and the postnatal period, and the potential problems which can occur due to catheterisation. This procedure is one I undertake and the article reassured me that I am basing my practice on the best available evidence |
| Why do you think the content made you feel like this? | The content of the article reassured me that my current level of understanding is good and up to date |
| What did you learn as a consequence of reading the article? | The article was more of a reminder of good practice and why the correct catheter size should be used. It also made me reflect on the personal nature of the procedure and that informed consent is fundamental, not only to this procedure but to all procedures when providing care for women |
Step 3: Reflective account: the impact/influence that the article has on your practice
| What have you done to complete the learning? | I have read the National Institute for Health and Care Excellence (2014) quality statement on urinary catheters and also the management of catheter care article in the reference list (Nazarko, 2010). Some women who have an epidural or a third- or fourth-degree tear may have an indwelling catheter for a longer period of time, therefore I would like to ensure I provide the best possible care and reduce the risk of infection and damage |
| What is the effect of your learning? | Reading this article made me reflect on the personal nature of the procedure and what it means. This led me to read the article in the reference list by Denis Walsh (2007) on the medicalisation of bladder care |
| What will you do differently as a result of reading the article? | I will use the article to discuss with students I work with the importance of good bladder care in pregnancy and labour. I will discuss the article by Walsh (2007) and ask them to read it, as it is reminder that catheterisation should not be a routine event and should not be undertaken as such. I will also discuss and be more proactive about pelvic floor exercises with women during pregnancy and the postpartum period |
National Institute for Health and Care Excellence (2014) Infection prevention and control. Quality statement 4: Urinary catheters. NICE, London Nazarko L (2010) Effective evidence-based catheter management: an update. Br J Nurs 19(15): 948–53. doi: 10.12968/bjon.2010.19.15.77689 Walsh D (2007) Medicalization of bladder care. British Journal of Midwifery 15(2): 87. doi: 10.12968/bjom.2007.15.2.22787
Turn to page 168 to see an example of how this clinical practice article might be used as material to support revalidation.

