In October 2013, two supervisors of midwives (SoMs) teams merged with the formation of Lewisham and Greenwich NHS Trust (LGT)—a total of 21 SoMs. Soon after, a ‘SoM clinic’ was created as a team initiative to facilitate one-to-one meetings between SoMs and women to discuss preferences for birth, to debrief about a previous birth, or both. Such meetings complemented standard midwifery practice, making sure the needs of women and their babies were the primary focus, and that midwives were working in partnership with women (Nursing and Midwifery Council (NMC), 2012) to create opportunities for them to engage actively with maternity services (NMC, 2008).
The meetings ensured that the midwives were fulfilling their role in advising and supporting women who use midwifery services; advocating for the right of all women to make informed choices, and providing additional advice to women who are experiencing difficulty in achieving care choices (NMC, 2008).
Previously, meetings were on an ad-hoc basis; reliant on the availabity of staff. This became increasingly difficult to organise as the profile of the team rose, and after the merge, the ‘Listening to Women’ initiative became increasingly popular. In 2016, 158 women were seen by the LGT SoM (94 were seen in 2014 and 150 in 2015).
The clinic—which, following the conversion of SoM to Professional Midwifery Advocate (PMA) is now called the ‘Listening Clinic’—has been expanded to all three Trust sites and is held close to the maternity unit. This provides space to accommodate the woman, partner, pram and/or toddler, and means that records, computer access and members of the multidisciplinary team are easily accessible. Some women are seen at home through preference or convenience. Each clinic has two appointments that last 1-1.5 hours; some discussions last longer and follow up meetings may be arranged to revisit preferences or after an outpatient appointment. Medical notes are obtained before meetings and are reviewed to inform discussions.
Terminology
There has been much discussion around the terminology used in appointments. SoM ‘birth plans’ have been viewed by some as an endorsement of a woman's choices and after discussion with senior managers and the SoM team, this was changed to ‘birth preferences’. It was felt that sharing women's preferences also represented what they felt they wanted to achieve rather than stipulating plans. Likewise, ‘debriefing’, with its connotations of psychology or counselling, in which SoMs were not trained, was changed to ‘birth discussions’. While not trained specifically to ‘debrief’, Axe (2000: 627) states that midwives ‘have up-to-date knowledge of midwifery and obstetric practice, access to the notes and have good listening and communication skills.’ The clinic provides the time and space for this.
Listening to women
As the 6Cs—Communication, Care, Compassion Competence, Courage and Commitment (Department of Health, 2012)—became better known during 2013 and early 2014, the LGT SoM team sought to embed them into their role, incorporating them into posters (Figure 1) ‘advertising’ the role of supervisors within the service, highlighting the SoMs' skills and interest in listening.

Shared experience
The LGT team is large (more than 400 midwives and 21 then-SoMs) and included a full time SoM post. The team's backgrounds were varied and experiences in practice diverse. Many of the SoMs held senior posts, some working clinically, and the team was—and still is—dispersed across all three sites. Equity of workload and networking opportunities were emphasised as being attributes of an effective SoM team (London Local Supervising Authority (LSA), 2013; NMC, 2014); the SoM clinic was commended as a proactive and supportive supervisory initiative. Face-to-face contact with users is invaluable. Emotions are often high and this exposure served to further motivate the SoM as an advocate in supporting choice, communicating preferences and addressing poor practice.
Referrals
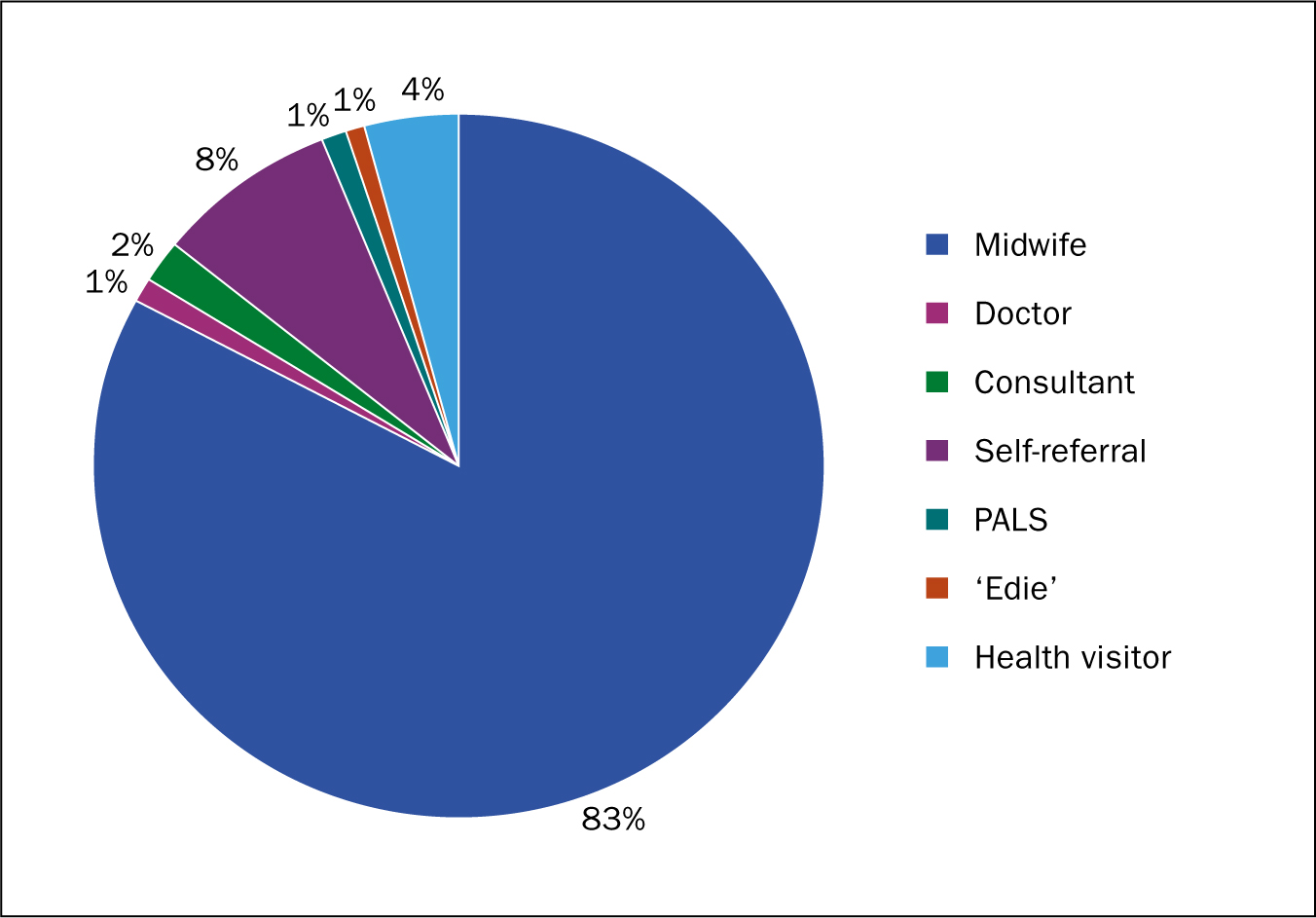
A referral form was developed and circulated to midwives, prompting essential information for contacting women at an appropriate time and for referrals to be triaged by the contact SoMs (CSoMs). This was shared with obstetricians, health visitors, family nurse practitioners and GPs with information about our service. The aim was to be accessible to all, and while the majority of referrals come from midwive s, we felt others were also well placed to offer our service (Figure 2). Our ‘virtual’ midwife, ‘Edie’, links via social media with women who may wish to discuss their experience or preferences for birth and signposts them to the now-PMA. Additionally the ‘direct access’ midwife has also referred women to the clinic; the Maternity Services Liaison Committees (MSLCs) have helped highlight the service and women have also been referred via Patient Advice and Liaison Services (PALs) and management where appropriate. Initially, the clinic seemed to be seeing more pregnant women wishing to discuss a previous birth experience; later women were accessing the service in a more timely manner after birth.
As stated by Espenhahn (LSA, 2016), the lay auditor in the LSA LGT report:
‘The number of referrals to SoMs from staff members of various disciplines shows how widely respected this support is within the Trust and the feedback from women who have had direct contact with a SoM is outstanding.’
Birth discussions: incorporating the 6 Cs
Through listening to women at birth discussions it became apparent to SoMs facilitating the clinic that each of the 6Cs were interrelated and that if one were to fail, perception of the other ‘C's by women and their families was detrimentally affected. It was evident that some members of staff did not communicate effectively; by being dismissive or not apparently listening, women felt that they did not care. This affected clients' perceptions of staff as competent, adding to feelings of being unsafe or vulnerable. Staff were then considered to be lacking in compassion by not apparently understanding their needs.
During meetings with women, the SoM (or PMA), can explain how staff do their best to communicate effectively, and explore reasons when on occasion they do not. We can strive to reinforce the competence of a midwife by reviewing their documentation and looking at practice; considering the management of the situation as a whole, and whether guidance has been followed.
The discussions add perspectives on situations that can lead to a better understanding of what happened and reduce feelings of trauma. At times, women have said that their own memory is blurred, having been focused on the intense experience. Having partners present for these discussions can help; they have their own perspective on the experience, but they may also have have been fearful for their partner or their baby's safety and wellbeing.
‘Seeing all the records from my labour to understand the order in which things happened and why. It really helped me to process the experience and gave me and my husband some sense of closure. I had quite a traumatic labour and the blood loss shocked my husband so it was good to work through things with him and the supervisor.’
By listening to experiences and acknowledging their feelings, we aim to restore their belief in our service's commitment to understanding what made a difference and how we will use their feedback to improve in future.
Courage has been required in undertaking these sessions, as they can feel quite uncomfortable and sometimes upsetting. Some of us have cried with women about their experiences and one SoM reported finding a hug has helped when a woman has shared a story. The hour's encounter can prove rewarding as well as challenging, and often leads to further work in ensuring the feedback is given sensitively and appropriately to the staff involved or to the managers responsible for the area. Further investigation into professional practice has been prompted at times, and we have also acted on constructive criticism from women:
‘Don't try to side with your team, keep neutral and don't try to make the woman feel as though you made the right choices—so to avoid it being taken further, be honest.’
Rewarding
Listening to a woman recount an important time of her life—and witnessing the emotions as they return, break the surface and move through the memories as they are recounted—is very rewarding. It can be a matter of moments before a woman you have never met before looks to the ceiling, or the floor and starts to cry as she revisits how it felt, and what she was thinking while in our care.
‘The supervisor was extremely helpful—very warm, friendly and understanding, and I felt that my thoughts and feelings were listened to and valued. I found it really useful to be able to go over my notes from my first birth and finally get some answers to questions and the experience that I hadn't understood.’
SoMs have felt they have made a difference ‘just by listening’ during the time they spent with women and their partners. This is not always vocalised at the time but may come later:
‘I'm sure you won't remember but I had a birth afterthoughts meeting with you nearly two years ago. My first daughter's birth was a traumatic experience for me and I found it very emotional talking through the notes with you. You really helped me to process it, I felt you really listened to me and explained it all in a way that helped me understand what happened .
I was pregnant at the time with daughter number two and terrified of a repeat experience … we went on to have a wonderful, intervention-free, planned home birth (on Christmas day!). Talking through the experience I had in hospital really helped me believe I could have a better birth experience second time around. Thank you very much; I'm sorry I didn't write sooner!’
Discussing birth preferences
Women were referred to the clinic to discuss their preferences for birth for numerous reasons. Once again, listening to their choices—and discussing why certain guidance was given and what midwives would be considering when caring for them—aimed to reinforce the message that we care.
We had the opportunity to risk assess in-depth, with a review of women's notes and an exploration of what they would want to happen and to do in certain circumstances. We have disseminated templates, detailing and reflecting our discussions with women as a means to sharing these preferences—and to give our colleagues the opportunity to ask questions or make suggestions themselves.
Further preparation, in terms of updating skills, preparing additional equipment or staff, was then considered. Printed copies were placed in the woman's handheld and hospital notes. Advice on what to be alert for was included—for example, in assessing a vaginal birth after caesarean (VBAC) woman labouring at home, midwives need to be observant for signs suggestive of scar dehiscence, with which community midwives may be less familiar.
It was suggested that if SoMs were seeing these women, they should be on call for them, or that by encouraging them to go ‘off guideline’ they were endorsing a choice that carries risks. In my experience, it was not that women were requesting something they did not need; rather they wanted to see what they could achieve. In listening to these wishes and communicating unbiased advice and information, we are personalising their care in line with Better Birth's (NHS England, 2016a:8) vision, ‘based around their needs and their decisions, where they have unbiased choice, informed by unbiased information.’
On occasion, women subsequently acknowledged that things may not have gone to ‘plan’ but they did get the opportunity to try and appreciated our support:
‘I thought I would let you know, that I had my baby girl on Sunday! Despite my BMI I had the loveliest experience giving birth, it was quick and very well handled by lady called Katie, there was no time for waterbirth though :)
Thank you again for giving me the chance and believing I could have a waterbirth and not crossing me off the list just because I didn't classify as capable :)’
Often, women simply wish to explore their options for births, and communicate their own reservations, preferences or desires.
Sharing the learning
Members of the SoM team were spread across the service, which facilitated the sharing of women's feedback through networking by the team, representation at meetings and within service design forums such as guideline groups, MSLCs and in training sessions. Themes from the Listening Clinic were a standing item on the monthly meeting agenda and new staff met with SoMs during their orientation. SoMs (now PMAs) also contribute to the maternity preceptorship programmes.
Seeing women more promptly after their babies' birth means timely feedback can be shared with the midwives involved. The midwives can more clearly remember the family, and this provides an opportunity to give their own account of what happened and reflect on the experience. Midwives are encouraged to save such feedback and reflections in their portfolios to contribute to their annual review, revalidation and appraisals.
Midwives who refer women for birth discussion or debriefs are encouraged to attend with the women if they can, to promote continuity within the antenatal period. This helps to develop their own understanding of the wider considerations and risk assessments involved in supporting women who may make atypical choices.
It became apparent through meeting with women that to listen to a woman telling her story was more powerful and motivating than a SoM feeding back to a midwife about their care—emphasising that what we say, and how we say it, is what makes the difference. We wanted to capture this and, after further discussion, some families have participated in creating DVD recordings of their stories, meaning we can share such emotive and powerful feedback with others. As SoMs were embedded in the service, and therefore expected to formally attend associated meetings, they presented their findings at numerous forums where themes were discussed. We plan to continue with this as PMAs. We have facilitated patient experience workshops, using the ‘Whose Shoes?’ toolkit, where women and their partners who have met with SoMs have participated and provided invaluable first hand accounts to a multi-professional audience.
Challenges
Through triaging referrals, it is apparent that a variety of issues referred to SoMs and now PMAs could potentially be resolved by confident, experienced midwives. There may be several factors affecting this, such as knowledge base or time constraints. The example and involvement of the SoM/PMA helps to develop the necessary skills and confidence in midwives to enable them to better support subsequent women.
The number of women seeking debriefing appears to be rising; this may be due to knowledge of our service and that of other trusts providing similar services, but we would hope the number would eventually decrease with overall improvements in care.
Staff caring for women who choose to birth outside of guidance do have some anxieties, and we would aim to help reduce these while balancing the support for women. This is addressed by involving midwives in discussions with women and meeting with individual midwives, their teams and management to discuss where further support can be provided e.g. with training and to review on-call provision.
Our work to date has focused predominantly on listening to women. In future we hope to capture and incorporate the experiences of fathers and family members more specifically to inform service development.
Our future and the new model of supervision
A recent online survey of women who had attended the clinic was positive and reflected well on their experience. As PMAs, we plan to continue seeing women through our clinic and referral system as we aim to ensure women feel listened to, and can access the information they need to make decisions about their care, and for staff to be supported to deliver women centred care in line with the vision of Better Births (NHS England, 2016a).
We plan to review our statistics further in relation to developing trends across sites to help us focus our future ambitions. This includes encouraging midwives to attend the clinic in future—they too may wish to access the opportunity to be heard and ‘debrief’ about an experience.
The new model for midwifery supervision incorporates restorative clinical supervision and so ‘aims to create space for thinking, feeling, reflecting and understanding’ (NHS England, 2016b). The presence of midwives attending with women enables exposure to the skills of the SoM/PMA and facilitates learning to support other women in the future; the aims of the new model being to equip professionals ‘to be familiar with and contribute to quality improvement, placing women and babies at the centre of care’ (NHS England, 2016b).
The functions of our clinic incorporate each of the Better Births (NHS England, 2016a) recommendations of personalised care, continuity of care, safer care, multi-professional working, postnatal and perinatal mental health.
‘I just wanted you to know how valuable the experience of your debrief and support was to me personally. I was traumatised by my birth and experience in hospital and I suffered serious depression which took me to some very bleak places mentally .
Without your support, I honestly believe I would still be ill instead of having gone on to make a full recovery and live a happy life again with my partner and my son.’
One local MSLC recently wrote to our Head of Midwifery to support our service in light of the review of supervision for the future:
‘We are hoping that the new arrangements recognise the need for a service such as this run by experienced midwives who are given protected time to listen and support women in this way .
As well as providing women with such good care, we are sure that this must save time and money further down the line in a multitude of ways.’
We have been able to demonstrate the effectiveness of our listening service to the senior management team through client feedback and user engagement in events. We are confident that we will be supported to continue with our efforts to improve patient experience and inform the service. There has been a recent reduction in complaints relating to attitude and we look forward to listening to more women in the future.
Conclusion
Listening to women through our ‘SoM Clinic’ initiative has been a rewarding experience for the staff involved and of benefit to the service as we have fed back what we have learned from the women and families we have been privileged to meet. The future of such initiatives should continue in line with the vision of Better Births (NHS, 2016a) and the continuation within the new A-EQUIP model of supervision.
‘I wanted to say a big thank you! for making the time to see me for a birth debrief last week. I found it tremendously helpful and exactly what I was after—felt very validated and like my feelings/thoughts around the birth were really listened to. It's really helped me to finally move on—hurrah!’

