Public Health England has estimated that 1 087 100 people in England, including 930 400 adults, have a degree of learning difficulty (Public Health England Learning Disabilities Observatory, 2015). However, there are no accurate numbers of parents accessing services (McGaw, 1997). Thurtle et al (2007) estimated that there could be 23 000–250 000 nationally; however, there are no more recent national statistics.
The Royal College of Nursing (RCN) (Rotherham, 2007) states that there should be a robust, flexible referral system for people with learning disabilities and a specialist or named midwife for disability. It sets out a group of standards to which all midwives and associated health professionals should work in order to provide effective care for patients with learning difficulties. This was underpinned by a Nursing and Midwifery Council (NMC) code of professional conduct in relation to people with disabilities that was produced by the Nursing and Midwifery Council (NMC). This code also stated that all Trusts should have a Disability Equality Scheme in place by 2000. However, this specific acknowledgement is no longer included in the latest version of the NMC Code (NMC, 2018).
Problem
My literature search showed that there were numerous definitions of learning difficulties, encompassing different manifestations in the individual.
This lack of an agreed definition creates an issue with research and literature searches, due to the differing language used in defining the term ‘learning difficulties’. In addition, if people do not refer to the same definition, there is a potential for an inequality of understanding, inclusion and care. The Department of Health (2001) provides a clear definition for health professionals. This definition states that to be classified as a having learning disabilities, a person must have:
‘A significantly reduced ability to understand new or complex information, to learn new skills (impaired intelligence), with a reduced ability to cope independently (impaired social functioning) which started before adulthood, with a lasting effect on development.’
Public Health England (2016) recommendations and the Equality Act [2010] state that people with learning disabilities should have reasonable adjustments made in order to improve engagement and reduce stress and anxiety. In practical sense this could mean:
Porter et al (2012) undertook a thematic analysis of the literature, in order to evaluate the accessibility and acceptability of resources from a professional and service user perspective. Their analysis concluded that there was a growing number of people with learning difficulties accessing care; however, few were identified by midwives in their study, therefore increasing the likelihood of prospective mothers with learning difficulties not receiving adequate antenatal care.
Background
The research showed no specific care pathway for women with learning disabilities, who are cared for as part of the mainstream care pathway (NICE, 2019). A learning disability affects the way a person understands information and how they communicate. This means they can have difficulty:
If no reasonable adjustments are made to accommodate the complex and diverse needs of women with learning disabilities, despite recommendations from Public Health England (2016), women may have fast-paced, high-information appointments, with very few opportunities for questions. These appointments can be distressing when women are asked to make informed decisions about their baby and their pregnancy, but have not taken in all the information that they need to make this choice. The role of antenatal appointments is to assist in decision-making, as well as assessing the health and wellbeing of the woman and baby. If there are no adjustments made for women with learning disabilities, it is difficult to provide women with accurate, factual and personalised care.
Most modern buildings now have adjustments for physically disabled patients to improve access and integration, but if health professionals do not know about reasonable adjustments for women with learning disabilities and do not offer them in healthcare settings, this could mean failing these women and their families, leaving the NHS open to litigation for not meeting basic legal requirements.
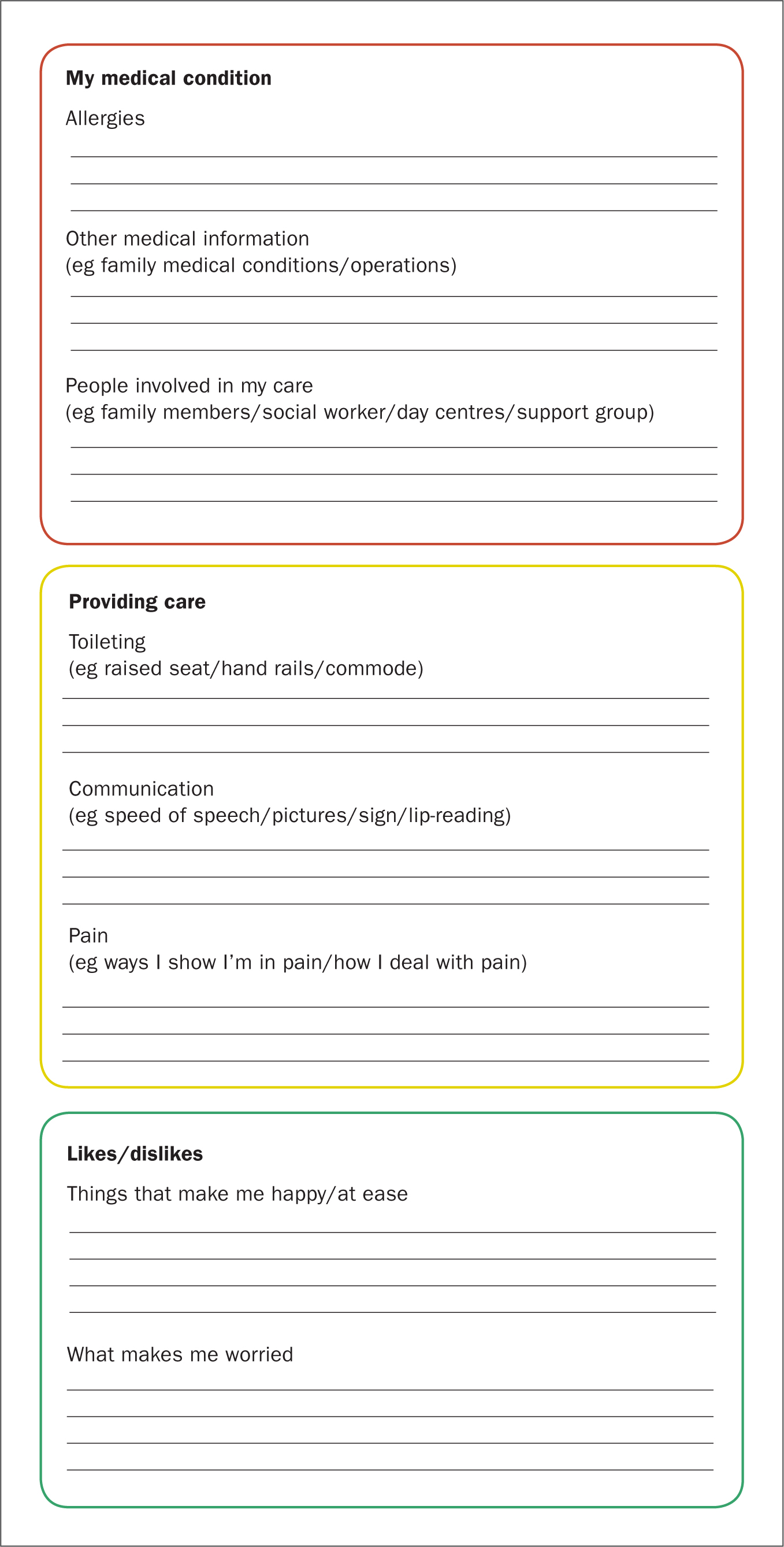
Trusts may use systems such as a ‘red, amber, green’ traffic light system to standardise and assist the delivery of all forms of care. This system can be used to categorise information by level of importance, so for example, crucial information such as allergies would be in red; important information such as sleeping habits would be in amber; and information such as relevant hobbies would be in green.
A lack of awareness may lead to a woman with learning disabilities being referred to a Trust's vulnerability team. This team is made up of specialist midwives who work with vulnerable women, such as those in the social care system, sex workers, women with a history of substance misuse and women with mental health issues. Due to the often high level of demand on these teams, contact with women with learning disabilities is governed by social care needs and co-ordination of multidisciplinary team members. It cannot improve engagement of the woman and her family with appointments, assist in identifying reasonable adjustments or prepare women for challenging situations. This service therefore offers very little extra support unless there are safeguarding issues identified. Not only is this often unnecessary for women with learning disabilities, but there is potential for an already stretched service that is not sufficiently trained to manage pregnant women with learning disabilities to see an increased workload.
Solution
My initial focus on the research internship programme was to create a ‘passport’ for pregnant women with learning disabilities. The aim of this document was to help health professionals to understand how an individual's learning disability affects their interaction with obstetrics and midwifery services. An individual care pathway would lead to better engagement with services, therefore leading to improve maternal and neonatal outcomes.
The passport is a document that can be completed by the antenatal team. It explores a range of aspects that could be important to the woman, such as food, hygiene, sleep, likes and dislikes; and consists of prompts as well as areas for detailed note-taking. This means that if someone needs bed guards and a single quiet room, the midwife could discuss this with the woman and her family, and reasonable adjustments could be made on admission. This passport would be taken everywhere with the patient, similar to the maternity notes, and updated when appropriate. This provides a way for health professionals to interact without having to re-question the woman, which reduces stress. The passport could also be adapted for general nursing use. A traffic light system is used on the passport, so that critical information such as name, address, medication, allergy status are red; important information such as food, hygiene and sleep are amber; and likes and dislikes are green. The document could easily be adapted to suit the systems in place at any particular Trust, in order to standardise care. An extract of the passport, providing examples of information in each colour category, is shown in Figure 1.
I would also like to develop an alternative care pathway for pregnant women with learning disabilities. This would identify a named midwife who would attend for appointments, meeting the Department of Health (2011) recommendations. This named midwife would attend scans with the woman, offer more frequent midwifery appointments and provide a slower pace of care that could be personalised to meet a woman's needs. This would provide more opportunities to discuss the complex aspects of pregnancy and would empower women to make their own decisions without being overwhelmed. This increased engagement with midwives, consultants and other health professionals could improve maternal and neonatal outcomes (National Maternity Review, 2016).
Evaluation
The research internship has enabled me to look at my own practice, and reflect on both the literature and the research journey. This time has also meant that I have been able to see how small changes can have a large impact for this group of women, standardising care and improving health outcomes.
A key theme in the literature was the need to provide timely information and improve multidisciplinary teamwork in order to reduce the likelihood of failings for parents with learning disabilities. Staff need to be educated on what reasonable adjustments are and the importance of making these adjustments to improve engagement and care delivery for women with learning disabilities. Altered care pathways, extra time and a slower pace of interaction would assist this engagement and the outcomes greatly; however there are costs and structural limitations to true patient-centred care. The lack of local data and actual service need from this client group compounds this issue. Some suggestions for how Trusts can improve their care are provided in Box 1.
Formal training as part of professional development or mandatory training on learning disability needs to be developed, as without this, staff may feel unable to provide the same standard of care as they do to women who are not identified as having a learning disability. Without reasonable adjustments, this often means that women with learning disabilities do not receive basic care. As a learning environment manager, I have also identified that students feel they do not have adequate training on this topic and feel they struggle to relate, connect and provide care to this group of women in particular.
More emphasis has been placed on a women-centred approach to care, creating a setting where women have an ability to actively partake in discussions and make informed choices (National Collaborating Centre for Women's and Children's Health, 2010). However, due to their complex needs, the voices of women with learning difficulties have been underrepresented. This further demonstrates how services are failing to meet the basic standards of care set out by the NMC Code (2018). This failure is not intentional; however, this lack of understanding, training and legal compliance by Trusts means that midwives are not aware of this obvious failing.
Conclusion
Disability is unique to the individual and can cross barriers of gender, age, sexual orientation, religion and race. Impairments can take many forms; some obvious and others covert in nature, varying between individuals.
All women should have the right to excellent, personalised, holistic and inclusive care. A comprehensive care pathway and integrated multidisciplinary passport unique to the individual could create the streamlined approach needed to provide excellent standards of care and better outcomes for women and babies.
Increased education on all aspects of learning disability, including the legal definition, what reasonable adjustments are and how they help should be provided, as well as a passport and an altered care pathway. This education must be for all members of the multidisciplinary team, so that all are able to assist women with learning disabilities and increase engagement, understanding and health outcomes for women and babies.

