Cardiac disease is the most common cause of indirect maternal death globally (Sanghavi and Rutherford, 2014; Lameijer et al, 2020; Knight et al, 2023). The complex physiological changes induced by pregnancy to meet the metabolic demands of the mother and the growing fetus (Taranikanti, 2018) can precipitate cardiac decompensation in women with pre-existing heart disease, increasing the risk of heart failure and arrhythmia, as well as having a negative impact on maternal and fetal outcomes (Ramage et al, 2019). Pre-pregnancy counselling and close monitoring during pregnancy and the puerperium are critical to the early detection of complications such as heart failure, arrhythmia and thromboembolic events.
In the UK, as in the rest of the world, 1 in 100 babies are born with congenital heart disease (Bakker et al, 2019). At least 97% will survive to adulthood, highlighting the need for long-term management strategies (Mandalenakis et al, 2020). With improved survival, an increasing number of women with congenital heart disease are opting to become pregnant and make up the majority of women seen in cardiac–obstetric clinics (Elkayam et al, 2016; Ramlakhan et al, 2021).
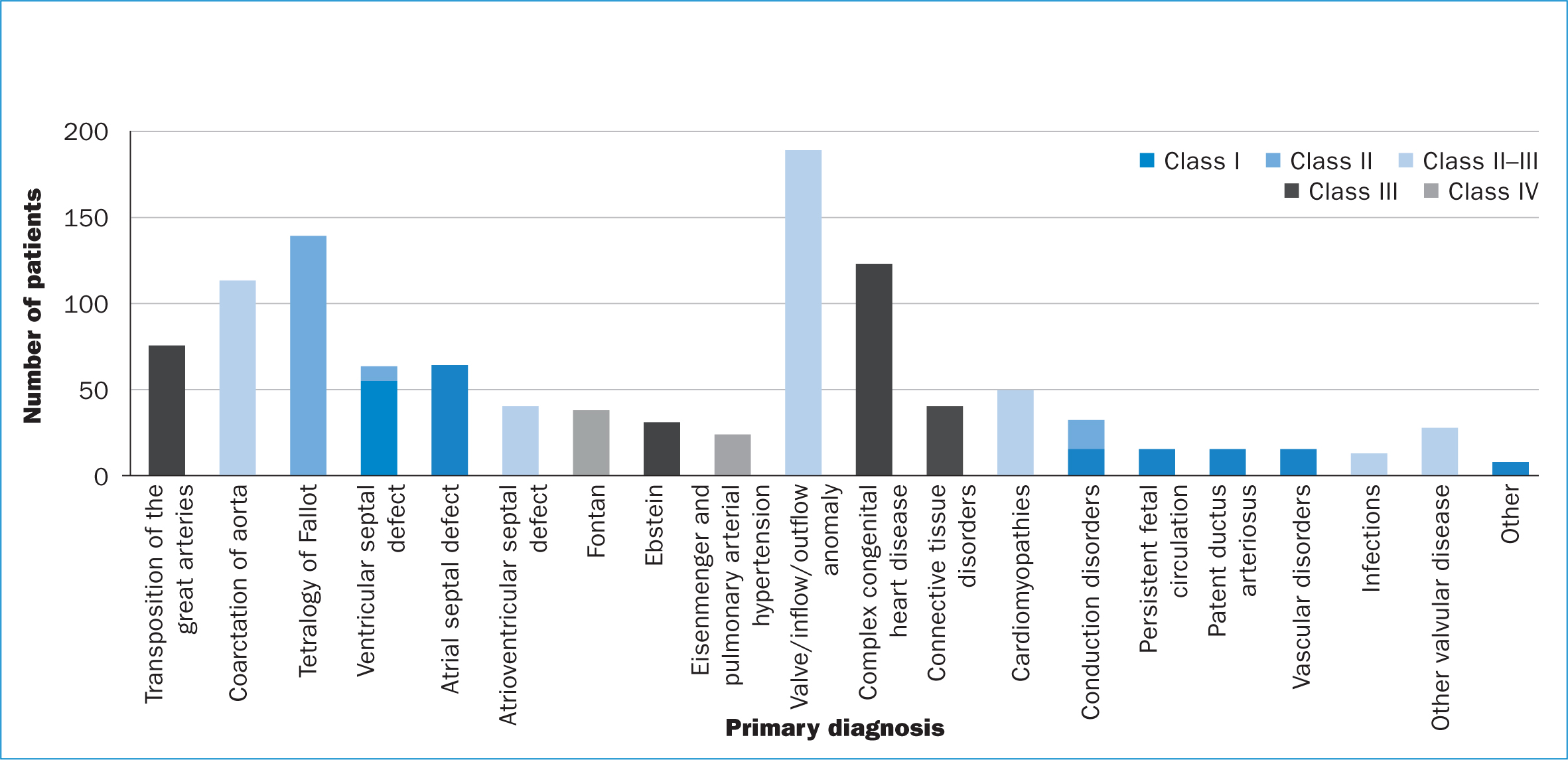
Pregnancy in women with complex congenital heart disease is associated with an increased risk compared with simple congenital heart disease lesions, independent of whether they were clinically stable at the time of conception (Canobbio et al, 2017). The modified World Health Organization classification categorises women into four pregnancy risk groups, classes I–IV (Essa et al, 2023). Class III is associated with a significant risk and class IV carries an extremely high risk of maternal mortality or severe morbidity; hence, in this category, pregnancy is strongly advised against (Canobbio et al, 2017).
The care of this emerging patient population needs careful assessment and management, starting with pre-pregnancy counselling and continuing through pregnancy and the puerperium (Canobbio et al, 2017). A fundamental role of the clinical nurse specialist is patient education and empowerment of pregnant women with congenital heart disease, providing comprehensive information about their cardiac condition, the potential impact of pregnancy on their cardiac and general health, and the importance of adhering to treatment plans. This education promotes informed decision making and enables patients to actively participate and engage in their care (Habibi et al, 2023). The UK confidential enquiries into maternal deaths highlighted that communication in a multidisciplinary team is required for accurate risk stratification, defining the correct intensity of care and reducing complications (D'Souza et al, 2015).
History and development of the joint tertiary cardiac/obstetric service
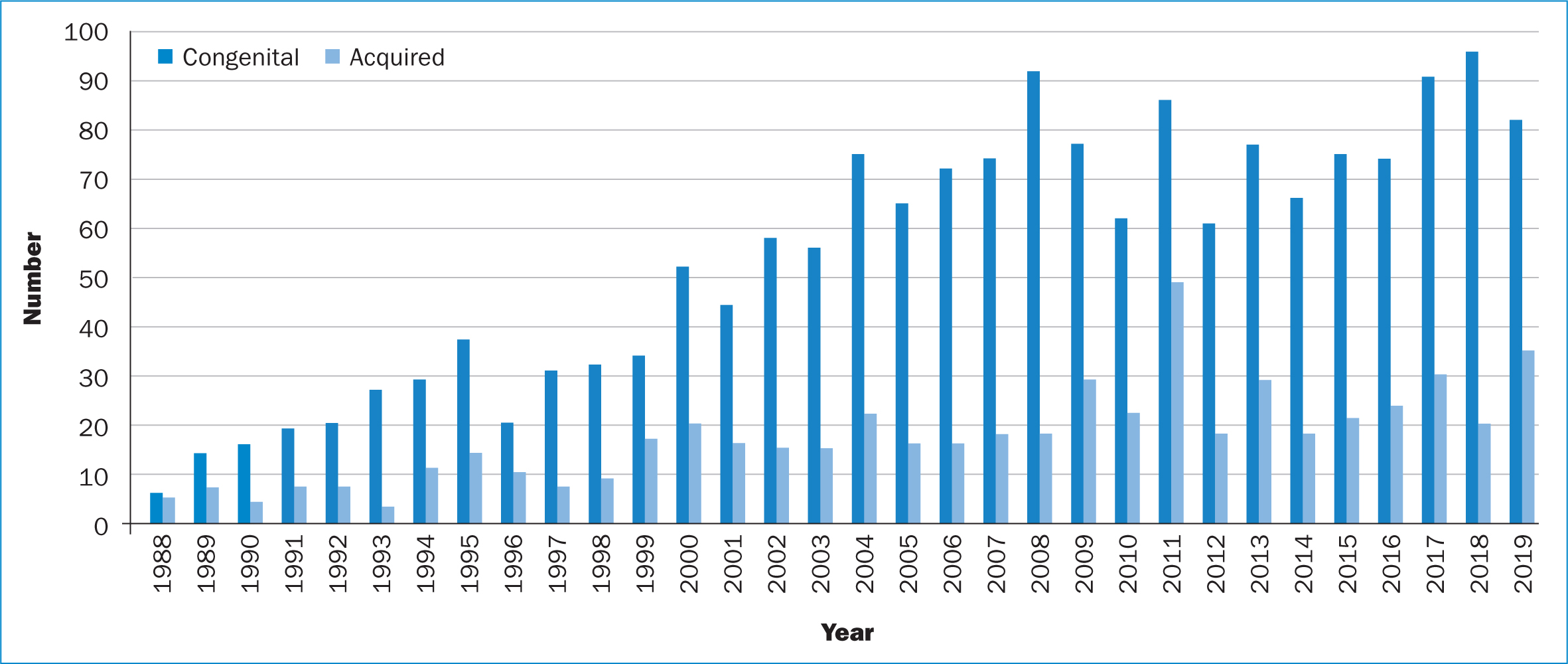
The joint cardiac and obstetric service at the Royal Brompton and Chelsea and Westminster Hospital, was established by Professor Phillip Steer and Dr Jane Sommerville in 1988. This was then expanded by Professor Michael Gatzoulis in 1999 to a face-to-face multidisciplinary clinic. The service has grown over the years (Figure 1).
The service now comprises two consultant obstetricians, three adult congenital heart disease consultant cardiologists and three adult congenital heart disease clinical nurse specialists who jointly run the weekly clinics on a rotational basis. Women are typically reviewed before 10 weeks' gestation and then at least once each trimester, depending on their complexity.
At each appointment, cardiac symptoms are reviewed, medication optimised and tests arranged. Regular assessments of cardiac function and fetal growth are performed and, when appropriate, fetal echoes requested. Individualised plans of care for the duration of pregnancy are made in the multidisciplinary team, and careful birth planning takes place with the input of consultant anaesthetists. This ensures a safe labour for mother and baby, which is especially important for women with WHO class III–IV conditions (Canobbio and Afshar, 2022).
Women are supported in their care choices and where possible, local birth is facilitated. This involves the team, supported by senior specialist trainees in obstetrics and adult congenital heart disease and consultant anaesthetists attending local multidisciplinary team meetings for birth planning and joint care for women who may live a considerable distance away. High-risk cases are also discussed at a weekly multidisciplinary meeting, with the goal of optimising patient care based on shared decision making.
Development of bespoke proforma for woman-centred care
The National Institute for Health and Care Excellence's (NICE, 2020) guidance states that it is the responsibility of the local team to develop protocols to ensure the regular assessment of pregnant women with an existing cardiac condition throughout their pregnancy. O'Kelly et al (2021) indicated that formal record-keeping tools should be developed to help identify individual women's risks and document how they will be managed. As such, the team developed two key proformas to be used throughout a woman's pregnancy.
Initial contact with the woman is triaged by one of the clinical nurse specialist teams using a proforma developed by the team to standardise the collection of patient data (Figure 2). It is used to identify any immediate clinical concerns, medication advice, symptom management and timing for initial clinical review. The service also supports women cared for by the inherited cardiac conditions team at the Royal Brompton Hospital, with referrals including patients with aortopathy, cardiomyopathies and conduction disorders. Women are also referred from outside centres (both obstetric and cardiology) at various gestations. The early collection of information is paramount to guiding appropriate antenatal care (Williams et al, 2021).
There is little published literature on recommendations regarding the development of a standardised triage sheet/proforma for the first contact with a pregnant women with congenital heart disease. Instead, the focus is on preconception counselling and ensuring that women who are aiming for conception are well educated on the potential risks and complications of pregnancy. By using the initial proforma, the clinical nurse specialist conducts a thorough assessment to identify potential risks and complications by identifying warning signs and intervening promptly to prevent exacerbations of cardiac symptoms.
Once triaged by the clinical nurse specialist, women are booked into the joint antenatal clinic at Chelsea and Westminster Hospital. A separate midwife appointment is arranged for the first antenatal booking, which involves an individualised assessment of the pregnant woman's needs for additional care and support during the pregnancy from the midwifery team (NICE, 2020).
During the clinic, a second proforma is used by the clinical nurse specialist to document the consultation. This is used to highlight medication changes, recent symptoms, investigation results, planned future investigations and follow-up. The clinical nurse specialist support the pregnant woman and her family by arranging investigations and being a named contact. Women who have been changed from oral anticoagulation to low molecular weight heparin will require regular monitoring to ensure they achieve therapeutic anti-factor Xa levels (Snape et al, 2018). The clinical nurse specialist liaises between local anticoagulation teams and haematology specialists to ensure this is arranged, as well as providing patient education on the importance of low molecular weight heparin and how to administer it. The second proforma is a crucial tool for documenting the progress of the pregnancy and facilitating continuity of care.
The role of adult congenital heart disease clinical nurse specialists
Preconception
As adolescents fully transition into adult services, continuing expert education on preconception care is vital. Contact with the clinical nurse specialist at transition and one-stop adult congenital heart disease clinics facilitates the clinical nurse specialist to proactively explore women's intentions to become pregnant in the future, offering personalised guidance through the process of pre-conception planning (Habibi et al, 2017). The clinical nurse specialist can then tailor their advice and education to the woman's individual needs, considering their current cardiovascular status and addressing modifiable risk factors, reviewing cardiac medications and discussing potential complications during pregnancy. This information helps a woman with pre-existing heart disease to make informed decisions about future pregnancies (Habibi et al, 2021). Figure 2 demonstrates the variety and complexity of patients seen in the preconception counselling clinic in the last 16 years, highlighting the important role it plays in educating women.
Promotion of health-protective behaviours and lifestyle modifications is another major component of pre-conception care, which benefits all women with congenital heart disease regardless of their plans to become pregnant (James, 2014). Modifiable risk factors should be addressed with women even before contemplating pregnancy, with studies showing that women who receive preconception advice are more likely to adopt healthier behaviours before pregnancy (Stephenson et al, 2014). These include stopping smoking and alcohol 3 months before pregnancy, keeping up to date on vaccinations, maintaining dental and gum health, reducing caffeine intake, treating anaemia and maintaining physical activity. In Australia, a study of women of preconception age found that those preparing for pregnancy put a focus on their general wellbeing as a motivator for change; areas such as nutrition and exercise were identified as more important than weight loss itself (Walker et al, 2022). Achieving an optimal weight and avoiding significant weight gain should also be emphasised (Charnley et al, 2024). The confidential enquiry into maternal morbidity and mortality between 2017 and 2019 noted that a high proportion of women who died were overweight or obese (Knight et al, 2023). With the increasing prevalence of obesity in developed countries (Sarma et al, 2021), this increases the chances of adverse events and should be discussed in a sensitive and tactful manner by the specialist nurse. Women who are overweight or obese should not be made to feel embarrassed or stigmatised, but equally need to recognise the risk posed by maternal obesity on pregnancy outcomes (Knight et al, 2021).
Folic acid supplementation before pregnancy (from 3 months before conception) is also advised, as this has been associated with reduced risks of fetal congenital heart disease (Mao et al, 2017). The recurrence risk of congenital heart disease in the offspring of women with congenital heart disease (without a genetic syndrome) is higher, between 3 and 5%, with higher rates in left sided lesions (10%), such as aortic stenosis, than the general population (D'Souza et al, 2015; Greutmann and Pieper, 2015), hence the importance of preconception folic acid.
Preconception counselling offers the opportunity for the review of a woman's medication and a comprehensive assessment of their cardiac function (Ramlakhan et al, 2021). Women with aortic coarctation, dilated or aneurysmal aorta and/or chronic hypertension should especially be counselled on the significance of blood pressure management and compliance with antihypertensive therapies. Certain drugs, such as angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, pose a risk of toxicity to the developing fetus (Wei et al, 2021). In early pregnancy, these are associated with an increased risk of malformations (Wei et al, 2021). In later pregnancy, there is increased risk of renal failure and oligohydramnios resulting in pulmonary hypoplasia (Wei et al, 2021). A clear plan to stop or switch these antihypertensive medications should be highlighted by the clinical nurse specialist and agreed upon with the woman and their cardiologist for any changes to be made either prior to conception or immediately after pregnancy is diagnosed. The comprehensive assessment of cardiac function allows optimisation prior to conception, either by adjusting medication or by surgical intervention. It also offers the opportunity for multidisciplinary team discussion (O'Kelly et al, 2021).
Regardless of their pregnancy plans, women are strongly encouraged to inform their congenital heart disease clinical nurse specialist as soon as pregnancy is suspected or confirmed so that they can be followed up in a specialised cardio-obstetric clinic. This is managed by the clinical nurse specialist to ensure the best outcomes for mother and baby. In high-risk pregnancies, the clinical nurse specialist can arrange more frequent check-ups and diagnostic tests to promptly identify and address any emerging issues (Habibi et al, 2023).
Risk of miscarriages and infertility
The risk of miscarriage in healthy women is estimated to be 12–15%, with 25% of pregnancies in women with congenital heart disease resulting in miscarriage, stillbirth or termination of pregnancy (Koerten et al, 2016). However, precise numbers are elusive because a high proportion of miscarriages during early pregnancy may go undocumented. Therefore, it is important to provide timely information to women on neonatal complications in terms of miscarriage or stillbirth.
The rate of termination of pregnancy in women with congenital heart disease is estimated to be around 5–8% (Koerten et al, 2016). In 2021, the WHO (2021) estimated that 73 million induced abortions occurred globally each year, with 29% of all pregnancies and 61% of unintended pregnancies ending in induced abortion. Termination of pregnancy is a difficult decision for women for a number of reasons such as socioeconomical, religious, health or psychosocial factors. There is little research into the reasons given by women for abortions, so it is difficult to draw comparison between the rates of termination of pregnancy in healthy women versus women with congenital heart disease.
The global prevalence of infertility is estimated to be 12.6–17.5% (Cox et al, 2022). The evidence regarding the prevalence of infertility in patients with simple to moderate congenital heart disease is mixed. In a retrospective study of 6000 women of childbearing age, Chien et al (2021) found that even patients with simple congenital heart disease had a higher risk of infertility. However, Udholm et al's (2023) study of over 8000 people (men and women) with congenital heart disease in Denmark found that the risks were the same as the normal population. Fertility is reduced in women with a Fontan circulation with causes possibly linked to hypoxia and coagulopathy (Zentner et al, 2016; Kim et al, 2020).
The options discussed in the clinic with women with congenital heart disease include in vitro fertilisation, with or without gestational surrogacy; however, the in vitro fertilisation procedure could pose risks during ovarian stimulation, egg retrieval and the post-procedure period (Kim et al, 2020). Therefore, because of the multiple risks, surrogacy may be a better option and should be discussed during pre-pregnancy counselling. The clinical nurse specialist provides advice to women with congenital heart disease and connects them to the relevant agencies.
Women with congenital heart disease who are advised against pregnancy, such as those with WHO class IV lesions, are counselled in a pre-pregnancy clinic with a full discussion about their options, including surrogacy and adoption. Women with single gene defects or a genetic syndrome (Di George's Syndrome) should be counselled about the availability of pre-implantation genetic diagnosis (Wander et al, 2023).
As the number of women with congenital heart disease becoming pregnant continues to grow (Elkayam et al, 2016), the demand for pre-conception care and counselling is rising. Adult congenital heart disease clinical nurse specialists with a special interest in pregnancy can support consultant cardiologists and obstetricians by providing pre-pregnancy counselling clinics, increasing the capacity of such services. Risk scores, such as the Cardiac Disease in Pregnancy Risk Score or ZAHARA, are available, but the WHO classification seems to be most consistent for women with congenital heart disease (van Hagen and Roos-Hesselink, 2020). Women in class I and II of the modified WHO classification are generally very low to low risk and could be suitable for counselling by adult congenital heart disease specialist nurses. Ultimately, close supervision and guidance from consultants with expertise in these specialities is crucial for this to be successful.
Antenatal care
During pregnancy, women need individualised care from a multidisciplinary team set up to minimise the risk of maternal mortality and morbidity (Sharma et al, 2021). NICE (2020) recognises that pregnant woman with pre-existing heart disease must have regular assessments throughout their pregnancy from a multidisciplinary team. The literature surrounding pregnancy in women with cardiovascular disease strongly focuses on the role of this cohesive team and highlights the need for unified care from pre-conception through to birth and postpartum (Cauldwell et al, 2016; Ramlakhan et al, 2021; Williams et al, 2021).
The Royal College of Obstetr icians and Gynaecologists (2016) maternity standards specify that women with complex medical conditions should have a named lead professional who works closely with the woman's named midwife. This is a role well suited to the adult congenital heart disease clinical nurse specialist, who may already have a close relationship with the woman. The clinical nurse specialist plays a key role in coordinating care and liaising with other healthcare professionals, such as a named midwife or local obstetric team, to ensure the best outcomes for mother and baby. In high-risk pregnancies, the clinical nurse specialist can arrange more frequent check-ups and diagnostic tests to promptly identify and address any emerging issues.
Pregnancy is a state that can make women feel increasingly vulnerable to psychosocial issues (Luna, 2019). This is recognised in the Royal College of Obstetricians and Gynaecologists (2016) maternity standards of metal health issues, which outline the need for service providers to have protocols for the early identification of women at risk. This underpins the importance of the clinical nurse specialist's role in pregnancy care, as a known healthcare professional giving confident and competent care to support and empower women (Griffiths et al, 2022). In addition, it is important to note that recent evidence suggests that up to 44% of women classed with high-risk pregnancies go on to suffer from mental health issues (Tsakiridis et al 2019). Therefore, the role of early identification of women at risk cannot be understated (Hamidia et al, 2022).
The compact nature of the adult congenital heart disease clinical nurse specialist team means that a woman is likely to see the same clinical nurse specialist regularly with the team working closely to discuss patient care, liaising with specialist midwives and highlighting any issues or concerns that need to be followed up. The impact of high-risk pregnancies on fathers is not to be underestimated. Fathers have reported stress and anxiety caused by a lack of communication from the medical team (Jackson et al, 2023). The clinical nurse specialist is also able to offer a family-centred approach by engaging, educating and supporting the pregnant woman and her partner, to enable all parties to feel included and supported during a high-risk pregnancy.
Antenatal fetal echocardiography screening
Ultrasound screening for the exclusion of congenital heart disease is offered to women in developed countries. If a severe abnormality is found, this gives the opportunity for a termination of pregnancy, and if a less severe lesion is identified, it allows the healthcare provider to organise appropriate neonatal care, reducing neonatal mortality (Bonnet, 2020). Tomek et al (2023) showed that when screening identified major congenital heart disease, this often resulted in a termination of pregnancy based on the parents' informed decision. The same study noted a higher termination rate in fetuses with univentricular heart morphology (Tomek et al, 2023).
Puerperium
After pregnancy, the clinical nurse specialist works to ensure cardiac follow up is arranged with appropriate tests and acts as a support for the woman (Habibi et al, 2023). The postpartum period is a critical phase for women with congenital heart disease, as their cardiac health can be influenced by the physiological changes associated with childbirth. Women with complex congenital heart disease are at risk of serious complications including haemorrhage (especially if they experience a caesarean section), heart failure, arrhythmia volume overload and thromboembolism (Lindley et al, 2021; Halpern et al, 2023).
For women with pulmonary hypertension, peri-partum cardiomyopathy or aortopathy, the postpartum period is particularly dangerous, as most deaths occur in the first month after birth, as a result of right heart failure, sudden death or thromboembolism (Singh et al, 2021). Women should be monitored closely after birth in an intensive care setting, to identify heart failure and the risk of rapid decompensation because of postpartum volume shifts as early as possible (Lindley et al, 2021). Maternal death is described as death from direct or indirect causes during or within 6 weeks of the end of pregnancy, but also could occur up to a year after the end of pregnancy (Knight et al, 2023).
Patients with congenital heart disease who have systemic right ventricular, left-sided obstructive lesions, single ventricle physiology or Eisenmenger syndrome are at the highest risk of heart failure postpartum (Deen et al, 2021).
Post-birth, women should be closely monitored because of rapid and significant hemodynamic adaptations, and require telemetry for a minimum of 24–48 hours, which should be individualised to each woman's needs. After discharge, women need to be in close contact with the clinical nurse specialist and be seen intermittently in the outpatient clinic for the first 6 months to be monitored for symptoms of heart failure (Canobbio et al, 2017).
One of the areas that pregnant women with congenital heart disease will discuss with the clinical nurse specialist is the effect of cardiac medication on breastfeeding. Breastfeeding is recognised as having a variety of benefits for both mother and infant, including physical, neurological and emotional, as well as promoting bonding (Byerley et al, 2022). Kearney et al (2018) supported the concept of individual risk assessment when considering breastfeeding for mothers on cardiac medication. They highlighted that the mother's care is the key priority, with breastfeeding compatibility being a secondary consideration. Women need to be supported in their choices of how to feed their babies, and women on high-risk medications should be counselled early regarding their options.
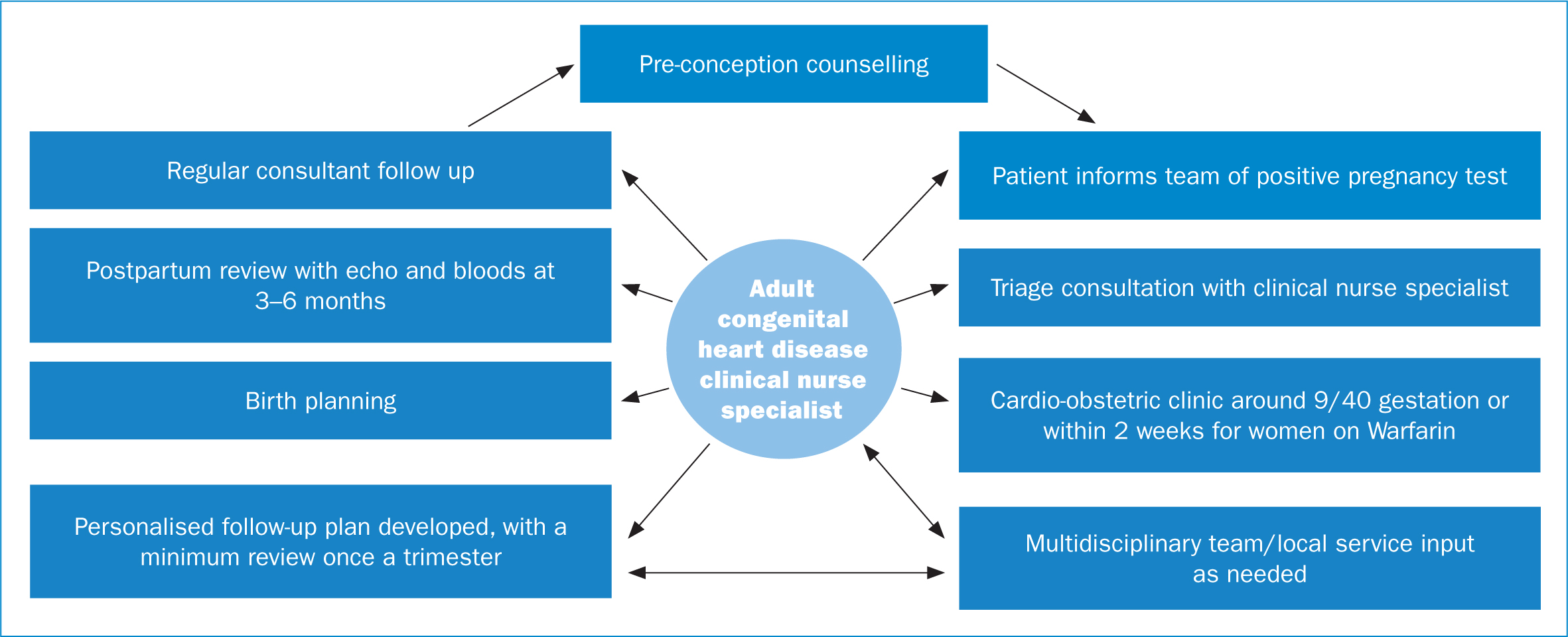
Providing individualised postpartum care is essential in ensuring the health and wellbeing of both the mother and newborn. The clinical nurse specialist plays a vital role in providing specialised care and support for pregnant women with congenital heart disease by ensuring a smooth transition from pregnancy to the postpartum period and safeguarding the health of the mother and baby. They will also ensure a smooth transition from the puerperium back into the usual cardiac service. The multidisciplinary cardio-obstetrics team need to collaborate closely to develop a birth and postpartum care plan for women with WHO class III–IV conditions (Canobbio and Afshar, 2022) (Figure 3).
Conclusions
Advances in medical and surgical care have dramatically improved the outlook for children with congenital heart disease. As the majority reach adulthood, and half of this population is women, pregnancy-related risks and advice on contraception should be discussed in a timely manner. The adult congenital heart disease clinical nurse specialist plays a critical role in all aspects of a woman's journey to motherhood, from initiating the discussion about contraception and pregnancy through to postpartum follow up. The clinical nurse specialist liaises with the cardio-obstetric team, including the adult congenital heart disease cardiologist, maternal–fetal medicine obstetrician, anaesthetist and other relevant subspecialties to optimise the care of this complex group of patients from pre-pregnancy to the postpartum period.
In this way, it is possible to anticipate and, if feasible, prevent complications that may arise during pregnancy, improving outcomes and allowing women with congenital heart disease to reach their full life potential. A team approach is paramount in achieving excellent care, and the clinical nurse specialist is central to this process.
Key points
- Women with congenital heart disease must be reviewed by a specialist in congenital cardiology and obstetrician during pregnancy.
- Pre-conception counselling is important for risk stratification and education for woman of reproductive age with congenital heart disease.
- The clinical nurse specialist liaises between the multidisciplinary team and named midwife to ensure safe and joined-up care.
- Close collaboration with local and specialist teams can facilitate woman-centred care.
- Birth planning is crucial to ensure a safe outcome for mother and baby.
CPD reflective questions
- What is the role of preconception counselling for woman who may have high-risk pregnancies?
- What is the role of the clinical nurse specialist in providing care to pregnant woman with congenital heart disease?
- Thinking of your clinical area, do you know who to refer to if you were caring for a woman with congenital heart disease?
- Thinking of your clinical area, do you feel you have effective proformas for highlighting woman with cardiac issues and how to manage them?


