For the majority of women childbearing is a normal life event. Physiological adaptations usually ensure a woman has a healthy pregnancy, childbirth and postnatal recovery. However, the increased cardiovascular reserves and other physiological changes in childbearing women can mask the sometimes inconspicuous signs of severe maternal illness. This can make recognition of impending maternal collapse difficult. ‘Women with serious illness, especially sepsis, may appear deceptively well before suddenly collapsing, often with little or no warning’ (Centre for Maternal and Child Enquiries (CMACE), 2011: 86). In addition, maternal wellbeing may be compromised in women of increased maternal age, obese women or women with complex medical conditions (Lee, 2014).
An early warning tool
It is important that midwives have the necessary effective tools available to aid clinical assessment and judgement when managing potentially life-changing complications in childbearing women.
Early warning scoring systems have been developed nationally following recognition and evidence that physiological abnormalities precede critical illness (Cullinane et al, 2005).
The use of an Early Warning Score (EWS) that is modified for use in pregnant and postpartum women will help in the early recognition, treatment and referral of women who have, or are developing, a critical illness, and is recommended. The rationale is that in many cases, early warning signs of impending maternal collapse go unrecognised (CMACE, 2011).
There is no national validated obstetric EWS system; however, there are a number of existing obstetric early warning charts in use across the UK and work is ongoing to develop a national obstetrics EWS (Royal College of Obstetricians and Gynaecologists (RCOG), 2011).
A national early warning score
The Royal College of Physicians (RCP) have recently recommended the use of a standardised national early warning score (NEWS) throughout the NHS for all adult patients (Royal College of Physicians (RCP), 2012). The report emphasises the importance of standardising clinical assessment of all adult patients across the NHS using a scoring sheet and standard physiological parameters. It is, however, clearly stated in the report that NEWS is not designed for use in pregnancy. The reason given is that the normal baseline for physiological parameters and the magnitude and character of the physiological response to acute illness differs in this group of patients (RCP, 2012). However, the RCP did not identify any specific gestation from which NEWS does not apply. In addition, there is no mention of the relevance of NEWS in the postpartum period.
A modified EWS tool for use in childbearing women
In Kettering General Hospital, a modified early obstetric warning system (MEOWS) chart is used from 20 weeks gestation when the woman is admitted to maternity wards. Many pregnancy-specific conditions occur after the 20th week, e.g. pregnancy induced hypertension and gestational diabetes (Stables and Rankin, 2005). In addition, physiological adaptations are likely to be more significant: ‘The changes in physiology seen in normal pregnancy mean that any scoring system may need to be modified for this group of patients as pregnancy progresses’ (Lewis, 2007: 241).
The MEOWS chart is used in the postnatal period up to the 6th week following childbirth. It is likely that physiological changes will have returned to a pre-pregnant state at this stage and most pregnancy-related illness will be resolved (Stables and Rankin, 2005).
The implementation of NEWS in the hospital for all adult non-obstetric patients prompted the urgent review of the modified obstetric tool. The RCP have highlighted the importance of a standardised approach when using an EWS system; the rationale being that a uniform approach to training and clinical use of the tool will ultimately improve patient safety (RCP, 2012). For this reason the Kettering General Hospital obstetric chart is modelled on the NEWS. Midwives will only encounter the MEOWS chart when caring for antenatal and postnatal women on maternity wards. Nurses, however, may be challenged with caring for obstetric patients on non-maternity wards, some of whom may be significantly at risk of deterioration. CMACE (2011: 11) state that: ‘It is equally important that these charts are also used for pregnant or postpartum women who are unwell and are being cared for outside obstetric and gynaecology services’.
Kettering General Hospital's MEOWS chart is contained within a booklet and is commenced on admission to hospital. The same booklet is used during subsequent admissions to hospital during the relevant pregnant and postnatal period. The booklet is maintained in the women's base notes folder. This enables midwives to see baseline observations and observe trends over time more easily at a glance. Tracking patient's clinical responses may indicate potential deterioration providing a trigger for escalation of clinical care. It will also provide guidance about the patient's recovery and return to stability thus facilitating a reduction in frequency and intensity of clinical monitoring and intervention (RCP, 2012).
The MEOWS chart should not be completed during established labour as a partogram should be used and clear guidelines already exist regarding frequency of observations and normal physiological parameters in labour (National Institute for Health and Care Excellence (NICE), 2007a). In Kettering General Hospital, the MEOWS score is documented on commencement of the partogram and then re-commenced following completion of the partogram.
Physiological parameters included in our MEOWS chart
The physiological parameters included in the MEOWS chart have been carefully selected to encompass all the standard observations required in a NEWS chart with the addition of those parameters specifically relevant to pregnant and postnatal women (Carle et al, 2013). The physiological parameters recorded on a NEWS chart are respiratory rate, oxygen saturation, temperature, systolic blood pressure, heart rate and conscious level. These form the minimum standard for routine monitoring of physiological observations set by the NICE (2007b).

Blood sugar can be recorded on the chart. The value is not mandatory and does not form part of the formal assessment; however, the result may be valuable to clinicians in some circumstances. Hyperglycaemia is one of the parameters included in the diagnostic criteria for sepsis (Dellinger et al, 2012). Urine output is relevant in some obstetric conditions and the inclusion in the chart may at least serve as a prompt to consider this feature.
Specific maternal observations that are recorded on the MEOWS chart are diastolic blood pressure, severity of pain, antenatal discharge and/or postnatal lochia and proteinurea.
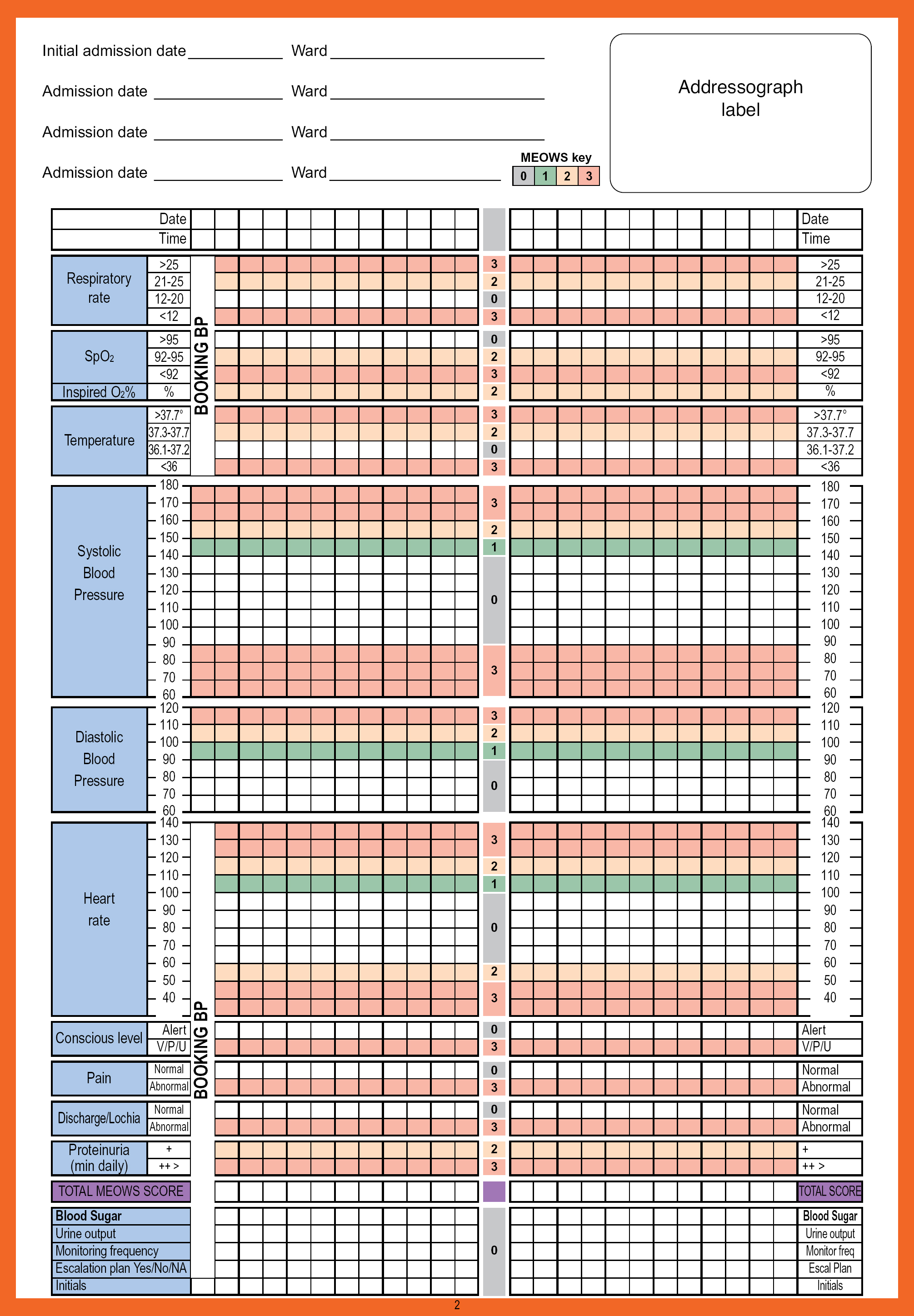
Diastolic blood pressure
Diastolic blood pressure is an important additional parameter used in the screening for and diagnosis of pre-eclampsia (NICE, 2008). There is reference in the MEOWS booklet to lowering the threshold for escalation where pre-eclampsia is suspected.
The first clinical observation recorded on the MEOWS chart is the booking blood pressure with the other physiological observations blocked. This enables clinicians to observe the booking blood pressure easily and monitor how it correlates with further readings.
Severity of pain
Pain is recognised as an important risk factor for severe maternal illness and mortality. Women who have unexplained pain severe enough to require opiate analgesia may have a severe problem and must be referred for specialist investigation and diagnosis. CMACE (2011) found that cardiac disease and other causes of death were missed when this sign was not identified. In the presence of pelvic sepsis, severe lower abdominal pain and severe ‘after pains’ that require frequent analgesia or do not respond to the usual analgesia are important symptoms. Severe pain just below the ribs is described as an important symptom of pre-eclampsia (NICE, 2010).
Antenatal discharge and/or postnatal lochia
Abnormal antenatal discharge is a symptom that may indicate an infection (CMACE, 2011). Abnormal and heavy postnatal bleeding is a significant cause of maternal morbidity and is likely to be linked to an infection (Marchant et al, 2002). Combined with other symptoms these findings may lead to a diagnosis of sepsis. The inclusion of this physiological parameter should encourage midwives and other clinicians to think about sepsis. There are frequent reminders throughout the MEOWS booklet to consider sepsis in all maternal cases where physiological parameters deviate from the norm.
Proteinurea
Urinalysis assessment of protein is included, the expectation being that urinalysis is performed as a minimum once daily when appropriate. The rationale is that midwives will consider pre-eclampsia (Milne et al, 2009).
Scoring physiological observations
The scoring system used on the Kettering General Hospital's MEOWS form is the same as NEWS. Physiological parameters which deviate from the norm are allocated a score. The score increases as deviation from the norm escalates. The final score then falls into one of three categories: a low, medium, or high score. Colour coding is used as it is in NEWS to give additional visual prompts to aid identification of abnormal physiological parameters.
The scores attributed to the standard physiological observations (respiratory rate, oxygen saturation, temperature, systolic blood pressure, heart rate and conscious level) differ from NEWS; with the exception of the conscious level assessment. The aim is to ensure the thresholds take into account not only the physiological differences between childbearing women and the general population but also given consideration to the specific areas of concern for this group of patients.
Diastolic blood pressure is scored taking into account the definitions of mild, moderate and severe hypertension outlined in NICE clinical guidance (NICE, 2010).
When assessing the level of pain a woman is experiencing, midwives use their clinical judgement and take into account the level of pain expected giving consideration to the full clinical picture. Where the level of pain is deemed to be abnormal or unexpected, the score attributed is high and should in itself prompt further investigation.
A similar theory applies when the midwife assesses the vaginal loss; clinical judgement is expected when determining if the vaginal loss is considered normal and expected or not.
Proteinurea is scored with an increase in score correlating to the level of protein detected on dipstick urinalysis.
Blood sugar and urine output do not contribute towards the final MEOWS score.
The recording of each necessary physiological parameter will not give specific readings but will give midwives a quick, clear indication of whether that observation is within normal limits. Midwives will record the exact physiological measurements in maternal notes when there is deviation from the norm.
Triggers for escalation
The trigger levels in the escalation algorithm contained within the MEOWS booklet are the same as NEWS. A low score is 1–4, a medium score is 5–6 and a high score is 7 or more. Any single score of 3 indicates an extreme variation from the normal, which is considered at least a medium score. The colour prompts are green for a low score, amber for medium and red for high scores (Figure 1).
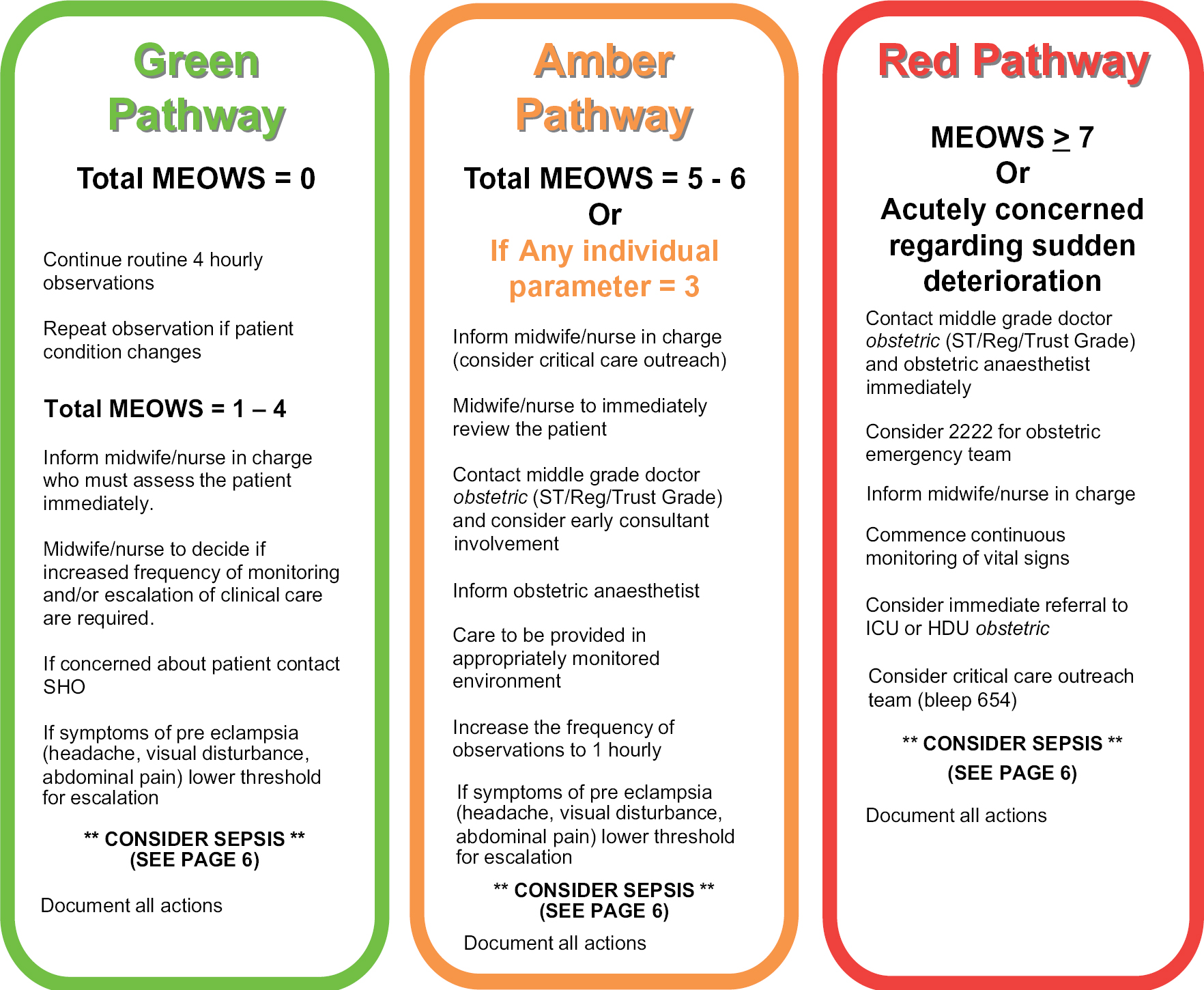
Escalation pathways
Identifying women who are at risk of, or who are developing, life threatening problems will only serve to improve outcome if early and appropriate intervention occurs. The escalation pathway in this MEOWS provides a guide to clinicians on the urgency of their response, the suggested level of support from the obstetric, medical, anaesthetic and midwifery team, the appropriate clinical location for the patient and the frequency of monitoring.
Kettering General Hospital has adopted a minimum standard of 4 hourly observations for all adult inpatients. To enable consistency, standardisation and for educational reasons our MEOWS adopts the same minimum frequency; however, there is scope for a reduction in frequency of observations to 12 hourly for obstetric patients who are deemed medically fit for discharge but may remain in hospital. Examples of these situations include the mother who remains in hospital for feeding support or whose infant requires hospitalisation. Midwives who exclude women from the minimum 4 hourly observations will document this decision on the front of the booklet. If the woman's clinical condition changes this exclusion can be cancelled and again recorded on the front of the booklet.
The associated local MEOWS guideline highlights the importance of compliance with other local policies which may require specific modifications to frequency of observations. Examples of this include women who are receiving a blood transfusion or who are post-obstetric anaesthesia. Kettering General Hospital's pathway contains additional prompts and guidance for clinicians suspecting sepsis or pre-eclampsia.
The MEOWS chart is a tool to aid clinical judgement and as with any EWS, midwives are expected to escalate concern when deemed necessary, sometimes irrespective of the guidance contained within the escalation pathway (Carle et al, 2013).
Kettering General Hospital's MEOWS booklet includes a locally agreed sepsis pathway, which follows recommendations from the Surviving Sepsis Campaign Care Bundles (Dellinger et al, 2012). Midwives and other clinicians are reminded to think about sepsis when referring to the escalation pathways. It is appropriate to incorporate sepsis guidelines in early warning tools as patients with severe sepsis can be significantly more unwell than they might appear (Parliamentary and Health Service Ombudsman, 2013).
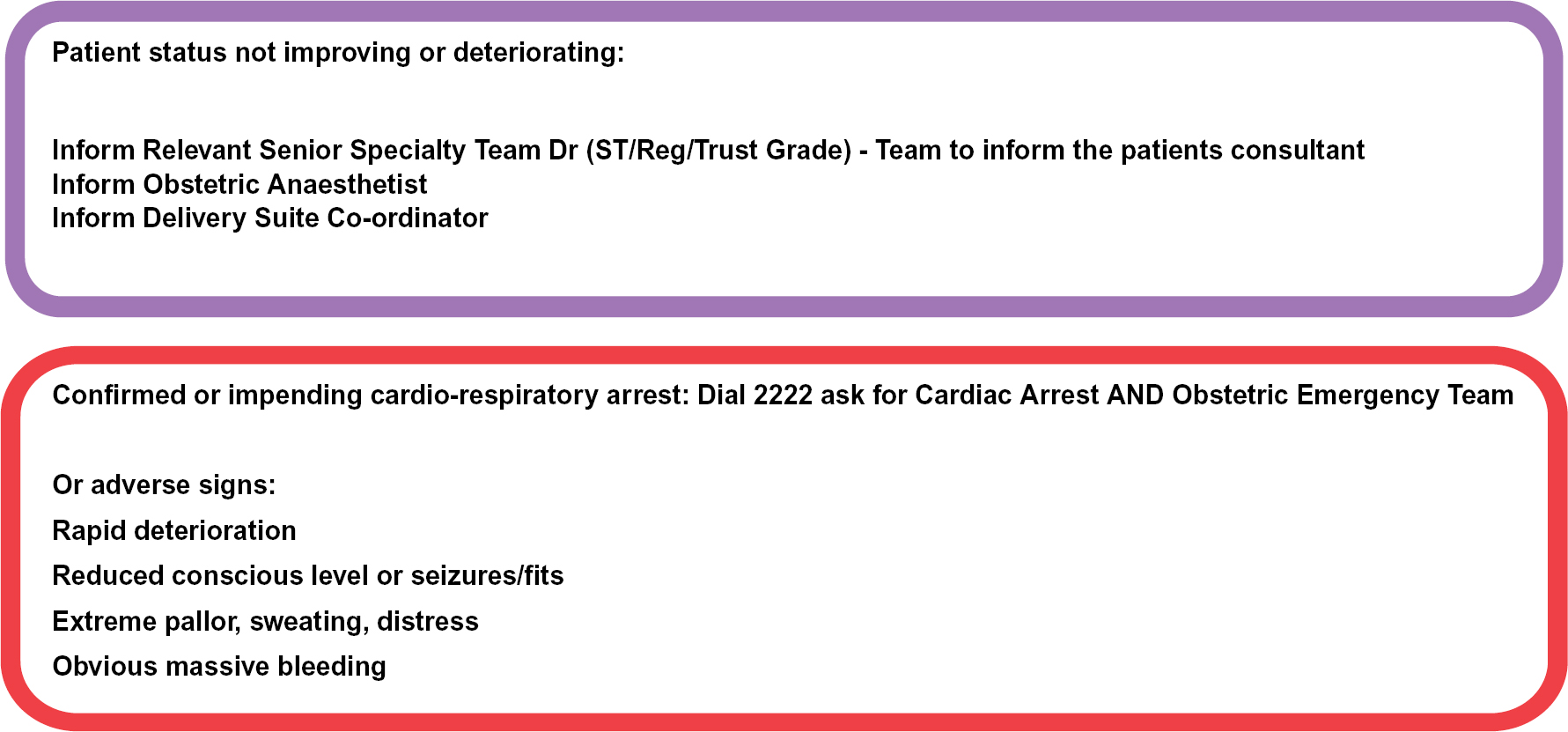
The competent and effective use of communication skills will be necessary when managing the unwell obstetric patient to ensure timely escalation of care and intervention. The Department of Health (DH, 2009: 7) state: ‘Organisations must ensure that their team have the necessary communication skills to convey the urgency of the situation and get immediate help from clinicians with appropriate knowledge and skills to ensure the patient receives optimum care’. Therefore, Kettering General Hospital adopted the communication tool, Situation Background Assessment Recommendation; SBAR. Guidance on how to use this tool in obstetrics is included within the MEOWS booklet.
Education
Midwives and other users of MEOWS will require robust training to ensure effective use of the system and clear, legible documentation of observations and interventions. The training needs of users at Kettering General Hospital are addressed using a variety of avenues. These include: vital signs skills assessment tools; inclusion in mandatory resuscitation training; cascade training; and online plus hard copy user guides. In addition, there are clear documentation standards attached to the MEOWS guideline. Staff caring for patients in any acute hospital setting should be competent in monitoring, measurement and interpretation of vital signs, equipping them with the knowledge to recognise deteriorating health and respond effectively to acutely ill patients (DH, 2009).
The skills of the team caring for the unwell obstetric patient will have an impact on patient outcome. Medical management and team work are important in the management of obstetric emergencies as if either are absent or lacking, morbidity and mortality may result (Dresang et al, 2010). In Kettering General Hospital, midwives along with other trained clinical obstetric practitioners such as doctors and theatre staff, can and do access the UK Resuscitation Council Immediate Life Support Course. The skills acquired during delivery of presentations, discussions, demonstrations, workshops and simulations are all related to the obstetric patient making it highly relevant. It is important that teaching is modified to reflect the practice area and educative needs of the target audience (Jennings, 2012).
When devising any MEOWS chart it is important to ensure that abnormal parameters do lead to a trigger prompting escalation. Ideally, the chart is highly sensitive to alerting the user when signs of impending illness are present. The number of precipitate alerts must be kept to a minimum however to ensure unnecessary escalation and intervention is not promoted. The Kettering General Hospital's MEOWS chart will be subject to scrutiny through internal audit.
Conclusion
Childbirth is a major life event and the physiological and psychological implications of serious illness on the woman and her family cannot be dismissed. While midwives strive to encourage and support normality for pregnant and postnatal women, equal importance must be assigned to identifying and acting on physiological changes occurring in women, which may indicate illness that without timely intervention can lead to significant maternal morbidity. A modified early obstetric warning tool provides a useful aid to clinical judgement during the assessment process and a structure to follow which should ensure timely and appropriate intervention when required. A locally devised tool can be modelled on the NEWS. The space available must be utilised effectively and enable clear and legible documentation.
The MEOWS booklet in Kettering General Hospital is commenced at 20 weeks gestation; however, it is possible that a modified EWS is applicable for all hospital admissions from pregnancy booking. Some physiological adaptations will be apparent early in pregnancy and may therefore warrant the use of a modified obstetric tool on admission to gynaecology wards.
There may be a place for adapting the principles of early warning scoring for use by community midwives. Childbearing women may develop illness outside hospital and a structure for assessment, intervention, escalation and appropriate referral is equally relevant in the community setting.
A validated national obstetric early warning tool would enable consistency and a necessary uniform approach to the assessment and management of potentially deteriorating childbearing women.

