Anaemia is a serious public health problem that affects 24.8% of the world's population and is the most prevalent nutritional deficiency disease worldwide (Gaillard et al, 2014; Gebreweld et al, 2018). It is a blood disorder in which the body does not have enough healthy red blood cells (Mayo Clinic, 2023). In pregnant women, it is defined as a haemoglobin concentration <11g/dL (World Health Organization (WHO), 2011). The WHO states that the prevalence of anaemia among pregnant women is 14% in industrialised countries and 51% in underdeveloped countries (Mangla and Singla, 2016). Approximately 65–75% of all anaemia cases in underdeveloped countries occur in India (Natekar et al, 2022). In sub-Saharan Africa, anaemia affects approximately 39% of women of reproductive age (WHO, 2017).
As a result of recurrent pregnancies and births, women of reproductive age are biologically more prone to anaemia (Gaillard et al, 2014). Socioeconomic factors can also put women at risk and vary by country (Balarajan et al, 2011; O'Neil et al, 2020). Risk factors for anaemia during pregnancy include younger maternal age (Rohim et al, 2018), low household income, low education, unemployment (Soh et al, 2015), late initiation of antenatal care (Jusoh et al, 2015), nonadherence to an iron supplementation regimen (Rosmawati et al, 2012), low serum ferritin levels (Gebreweld et al, 2018), being in the second or third trimester, high parity (Za et al, 2017) and glucose-6-phosphate dehydrogenase deficiency (Engwa et al, 2017). Over 400 million people worldwide are affected by this deficiency, which is an X-linked incomplete dominant inheritance disorder of red blood cell enzymes and one of the most common causes of haemolytic anaemia (Richardson and O'Malley, 2022).
Glucose-6-phosphate dehydrogenase activity is one of the most common tests administered when pregnant women attend antenatal care for the first time. The WHO glucose-6-phosphate dehydrogenase activity classification ranges from undetectable (<1% enzyme activity), partially detectable (≤60%) to normal or increased (>60%) (Gautam, 2016). Pregnant women who are glucose-6-phosphate dehydrogenase deficient are likely to experience oxidative stress when they contract certain infections (beta-hemolytic streptococci, rickettsial disease, viral hepatitis, salmonella, Escherichia coli and influenza A), take certain medications (sulfur-containing drugs) or eat certain foods (fava beans) (Richardson and O'Malley, 2022). These experiences may cause a reduction in glutathione, rendering red blood cells prone to oxidative damage and, ultimately, haemolysis or anaemia (Richardson and O'Malley, 2022).
There are differences in regional haemoglobin concentration thresholds for diagnosing anaemia in the general population, including pregnant women. In Ghana, the standard methaemoglobin reduction technique (Cheesbrough, 2005) is used to classify test outcomes into normal, partial defect and full defect for enzyme activity. The WHO (2021) recommends a minimum threshold of 10.5g/dL for anaemia diagnosis in the second trimester of pregnancy; however, Ghana uses a threshold of 11.0g/dL across all three trimesters (Ghana Ministry of Health, 2017).
Pobee et al (2021) reported that the prevalence of anaemia (classified as Hb<11g/dL) among pregnant women in Ghana was 37%, 63% and 58% in the first, second and third trimesters, respectively. Simpong et al (2023) reported the prevalence in Ghana was moderate in the first (36.4%) and second trimester (31.6%) and severe in the third trimester (68.0%). The study classified anaemia according to WHO trimester-specific haemoglobin cut-offs (Young et al, 2019). These findings suggest that anaemia may progress from mild to severe later in pregnancy.
Antenatal care is critical for allowing access to health promotion education and preventive health services for women and fetuses, as well as establishing relationships with midwives and healthcare professionals. It also allows testing for concerns such as glucose-6-phosphate dehydrogenase deficiency (Ghana Ministry of Health, 2017). In the case of complete or partial deficiency, women are advised to avoid sulfonamide medications (such as sulfadoxine-pyrimethamine, a prophylactic antimalarial) and certain foods to avoid haemolysis (Owusu et al, 2015).
Anaemia and glucose-6-phosphate dehydrogenase deficiency are both medical disorders that can have serious clinical consequences for pregnant women. According to data from the internally published half-year review of the Central Region Health Service in 2023, 27% of all pregnant women attending antenatal care in the Cape Coast district were anaemic. In the past 3 years, potential consequences of anaemia have been reported in high numbers at Cape Coast Metropolitan Hospital, including stillbirths, spontaneous abortions and low birth weight (Table 1). Glucose-6-phosphate dehydrogenase deficiency can induce haemolytic anaemia, leading to fatigue, weakness and shortness of breath. Understanding the prevalence of this deficiency in pregnant women is critical for ensuring that proper care and birth outcome measures and policies are improved.
| Indicator | 2020 | 2021 | 2022 |
|---|---|---|---|
| Stillbirth | 18 | 13 | 11 |
| Postpartum haemorrhage | 0 | 1 | 0 |
| Spontaneous abortion | 49 | 30 | 57 |
| Low birth weight | 53 | 103 | 39 |
| Antenatal care attendance | 5917 | 5344 | 5448 |
| Antenatal care registrants | 774 | 719 | 686 |
Taken from: internal district records
This study assessed the association between anaemia and glucose-6-phosphate dehydrogenase deficiency among pregnant women at the Cape Coast Metropolitan Hospital in 2022. The aims were to determine the prevalence of anaemia at registration (up to 13 weeks) and at 36 weeks' gestation among pregnant women who attended antenatal care, to determine the prevalence of glucose-6-phosphate dehydrogenase deficiency in this population, and to determine if there was a significant link between anaemia, glucose-6-phosphate dehydrogenase deficiency and other predictors.
Methods
This facility-based cross-sectional study extracted data from antenatal care registries at the Cape Coast Metropolitan Hospital in the Central Region of Ghana, analysing records for women from 1 January–31 December 2022. The attendance at antenatal care in 2022 was 5448 pregnant women, of which 686 were officially registered (Table 1), meaning they completed antenatal care at the hospital.
Study population
The study population was all antenatal care registrants who attended care and gave birth at Cape Coast Metropolitan Hospital in 2022. Of the 686 pregnant women registered, 369 were included in the study, as they had complete data, were registered before 13 weeks' gestation and attended antenatal care at the hospital.
Data collection
An Excel sheet of required variables was used to collect data from the antenatal care registers. Collected variables were haemoglobin concentration at first visit and at 36 weeks' gestation, presence of glucose-6-phosphate dehydrogenase deficiency, occupation, ethnicity, education, residence, marital status, weight, height, parity, gravidity and sickle cell status. Missing data were traced to the Light-Wave Health Information Management System platform, an intranet electronic software for capturing patient demographics, history and treatment plans, as well as requesting diagnostic tests, receiving results and referring patient.
Data analysis
Anonymised data were entered into a Microsoft Excel sheet and exported to the Statistical Package for Social Sciences (version 27.0). Women were characterised as either ‘not anaemic’ (Hb> 11g/dL) or ‘anaemic’ (<11g/dL). Anaemia was classified as mild (Hb 9–10.9g/dL) or moderate (Hb 7–8.9g/dL) (Goonewardene et al, 2012). Glucose-6-phosphate dehydrogenase was classified as normal, partially deficient, or deficient based on the methaemoglobin reduction technique (Cheesbrough, 2005).
Bivariate analysis was performed using the Chi-squared independence test to determine whether anaemia and independent factors were associated. All variables found to influence anaemia were then included in multiple logistic regression analysis. Factors were deemed statistically significant if P<0.05.
Ethical approval
This study was conducted under the mandate of the Public Health Division of the Ghana Health Service to investigate public health emergencies. The Central Region Health Directorate granted consent and waived the need for ethical approval for this study as it used secondary data and aimed to improve patient management outcomes, making it exempt from Ghana Health Service institutional review board approval. In addition, it was deemed part of efforts to find solutions to pregnancy-related complications resulting from anaemia. The Regional Health Directorate and Cape Coast Metropolitan Hospital Medical Director were asked for their consent to use the data. Data were anonymised and only study team members had access to the password-protected data generated by this study.
Results
The records from 369 pregnant women with a mean age of 28.23 ± 6.47 years were included. Their ages ranged from 14–45 years. The majority of the sample were single (60.4%), employed (53.9%) and from the Fante ethnic group (86.7%). Full sociodemographic data are shown in Table 2.
| Variable | Frequency, n=369 (%) | |
|---|---|---|
| Age (years) | <20 | 39 (10.6) |
| 20–24 | 69 (18.7) | |
| 25–29 | 99 (26.8) | |
| 30–34 | 99 (26.8) | |
| 35–39 | 48 (13.0) | |
| ≥40 | 15 (4.1) | |
| Marital status | Single | 223 (60.4) |
| Married | 146 (39.6) | |
| Education | Junior high school | 146 (39.6) |
| Senior high school | 156 (42.3) | |
| Tertiary | 67 (18.2) | |
| Employment | Employed | 199 (53.9) |
| Unemployed | 170 (46.1) | |
| Ethnicity | Fante | 320 (86.7) |
| Ga | 3 (0.8) | |
| Ewe | 17 (4.6) | |
| Hausa | 28 (7.6) | |
| Ashanti | 1 (0.3) |
Anaemia
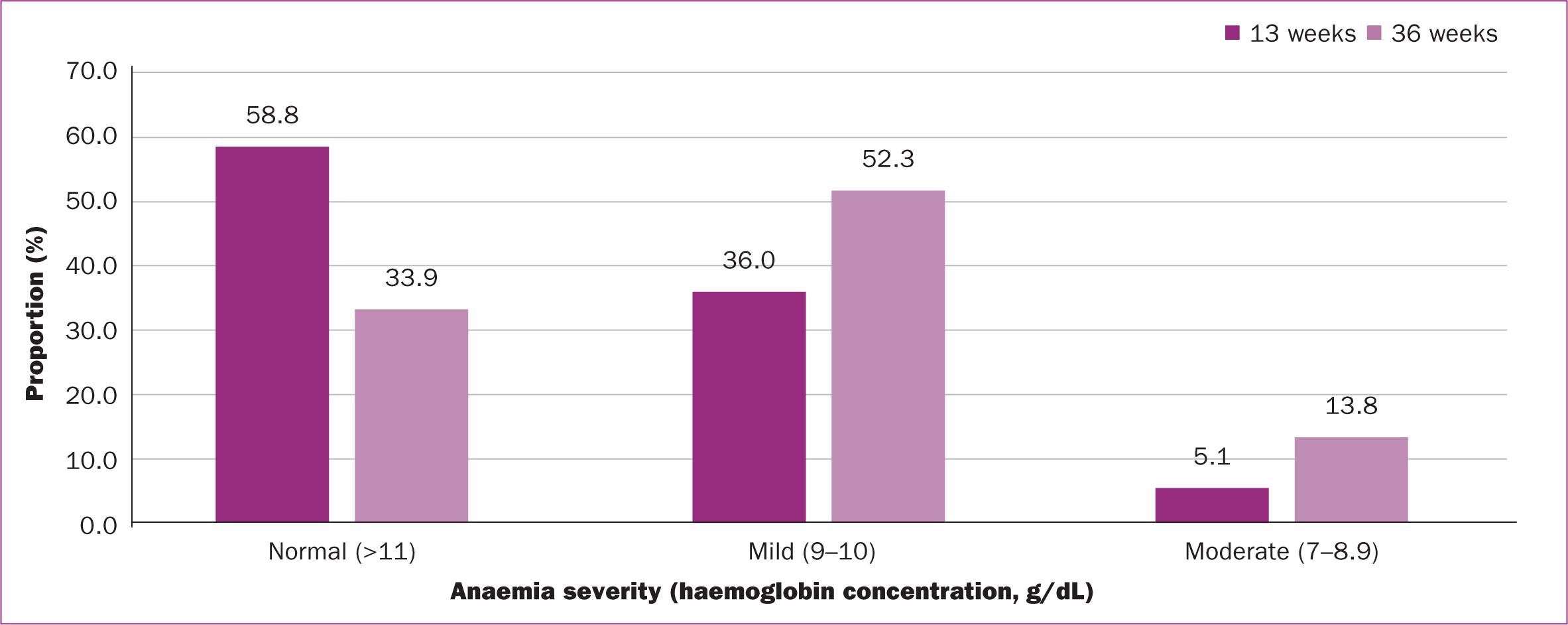
The prevalence of anaemia was 41.2% for women at 13 weeks' gestation and 66.7% at 36 weeks. Between 13 and 36 weeks, the prevalence of mild anaemia increased 1.45 times, while moderate anaemia increased by 2.7 times (Figure 1). The mean Hb concentration at 13 weeks was 11.19 ± 1.34g/dL. At 36 weeks, the mean Hb concentration was 10.33 ± 1.11g/dL.
Glucose-6-phosphate dehydrogenase deficiency
Glucose-6-phosphate dehydrogenase deficiency (partial or full) was found in 29.8% of pregnant women; 39.1% of those with this deficiency were anaemic at 13 weeks, and 62.7% were anaemic at 36 weeks. There was no statistically significant association between anaemia and glucose-6-phosphate dehydrogenase deficiency at 13 (P=0.803) or 36 weeks (P=0.482).
Association between anaemia and covariates
Several factors were significantly associated with anaemia (Table 3), including employment status among those at 36 weeks (P=0.003), maternal age among those at 13 weeks (P=0.011) and gravidity among those at 36 weeks (P=0.013).
| Variable | Anaemia | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 13 weeks | 36 weeks | ||||||||
| Not anaemic | Anaemic | X2 | P value | Not anaemic | Anaemic | X2 | P value | ||
| Glucose-6-phosphate dehydrogenase deficiency | Normal | 150 (40.7) | 109 (29.5) | 0.44 | 0.803 | 82 (22.2) | 177 (48.0) | 1.46 | 0.482 |
| Deficient | 67 (18.2) | 43 (11.6) | 41 (11.1) | 69 (18.7) | |||||
| Marital status | Single | 136 (36.9) | 87 (23.6) | 1.11 | 0.293 | 78 (21.1) | 145 (39.3) | 0.69 | 0.408 |
| Married | 81 (22.0) | 65 (17.6) | 45 (12.2) | 101 (27.4) | |||||
| Education | Junior high school | 82 (22.2) | 64 (17.3) | 3.45 | 0.327 | 53 (14.4) | 93 (25.2) | 6.29 | 0.098 |
| Senior high school | 98 (26.6) | 58 (42.3) | 56 (15.2) | 99 (26.8) | |||||
| Tertiary | 37 (39.4) | 30 (8.1) | 14 (3.8) | 53 (14.4) | |||||
| Employment | Employed | 126 (34.1) | 73 (19.8) | 3.63 | 0.057 | 53 (14.4) | 146 (39.6) | 8.73 | 0.003 |
| Unemployed | 91 (24.7) | 79 (21.4) | 70 (19.0) | 100 (27.1) | |||||
| Ethnicity | Fante | 188 (51.0) | 132 (35.7) | 9.20 | 0.239 | 113 (30.7) | 207 (56.1) | 6.25 | 0.511 |
| Ga | 1 (0.3) | 2 (0.5) | 1 (0.3) | 2 (0.5) | |||||
| Ewe | 9 (2.4) | 8 (2.1) | 3 (0.8) | 14 (3.8) | |||||
| Hausa | 18 (4.9) | 10 (2.7) | 6 (1.6) | 22 (5.9) | |||||
| Ashanti | 1 (0.3) | 0 | 0 | 1 (0.3) | |||||
| Age (years) | < 20 | 14 (3.8) | 25 (6.8) | 14.77 | 0.011 | 13 (3.5) | 26 (7.0) | 8. 48 | 0.132 |
| 20-24 | 43 (11.7) | 26 (7.0) | 27 (7.3) | 42 (11.4) | |||||
| 25-29 | 53 (14.4) | 46 (12.5) | 39 (10.6) | 60 (16.3) | |||||
| 30-34 | 68 (18.4) | 31 (8.4) | 22 (6.0) | 77 (20.9) | |||||
| 35-39 | 31 (8.4) | 17 (4.6) | 16 (4.3) | 32 (8.7) | |||||
| ≥ 40 | 8 (2.2) | 7 (1.9) | 6 (1.6) | 9 (2.4) | |||||
| Sickle cell status | Negative | 193 (52.3) | 129 (35.0) | 1.33 | 0.248 | 105 (28.5) | 217 (58.5) | 0.60 | 0.440 |
| Positive | 24 (6.5) | 23 (6.2) | 18 (4.9) | 29 (31.3) | |||||
| Gravidity | 1 | 47 (12.7) | 38 (10.3) | 3.14 | 0.208 | 18 (4.9) | 67 (18.2) | 8.64 | 0.013 |
| 2 | 50 (13.6) | 44 (11.9) | 39 (10.6) | 55 (14.9) | |||||
| ≥ 3 | 120 (32.5) | 70 (19.0) | 66 (17.9) | 124 (33.6) | |||||
| Parity | ≤ 1 | 120 (32.5) | 99 (26.8) | 3.58 | 0.167 | 76 (20.6) | 143 (38.8) | 5.15 | 0.076 |
| 2 | 46 (12.5) | 25 (6.8) | 16 (4.3) | 55 (47.3) | |||||
| ≥ 3 | 51 (13.8) | 28 (7.6) | 31 (8.4) | 48 (13.0) | |||||
Table 4 outlines the results of the multiple logistic regression analysis. Glucose-6-phosphate dehydrogenase deficiency was not significantly associated with anaemia in pregnant women at 13 or 36 weeks. Women who were older (P=0.024) or single (P=0.009) were significantly less likely to have anaemia at 13 weeks. Women who were unemployed (P=0.001) or had higher gravidity (P=0.014) were significantly less likely to have anaemia at 36 weeks.
| Variable | Anaemia | ||||||
|---|---|---|---|---|---|---|---|
| 13 weeks | 36 weeks | ||||||
| Crude odds ratio (95% confidence interval) | Adjusted odds ratio (95% confidence interval) | P value | Crude odds ratio (95% confidence interval) | Adjusted odds ratio (95% confidence interval) | P value | ||
| Glucose-6-phosphate dehydrogenase deficiency | Normal | 1 | 1 | 1 | 1 | ||
| Deficient | 1.170 (0.740–1.849) | 0.847 (0.528–1.357) | 0.489 | 1.236 (0.774–1.975) | 0.781 (0.477–1.280) | 0.328 | |
| Marital status | Married | 1 | 1 | 1 | 1 | ||
| Single | 0.797 (0.478–1.217) | 0.451 (0.249–0.819)* | 0.009 | 0.828 (0.530–1.294) | 0.764 (0.411–1.419) | 0.394 | |
| Education | Junior high school | 1 | 1 | 1 | 1 | ||
| Senior high school | 0.758 (0.478–1.202) | 1.083 (0.578–2.028) | 0.804 | 1.018 (0.636–1.628) | 0.620 (0.324–1.185) | 0.148 | |
| Tertiary | 1.039 (0.580–1.859) | 1.764 (0.744–4.185) | 0.198 | 2.157 (1.094–4.253) | 1.385 (0.537–3.575) | 0.500 | |
| Employment | Employed | 1 | 1 | 1 | 1 | ||
| Unemployed | 1.498 (0.987–2.274) | 1.615 (0.733–3.559) | 0.235 | 0.519 (0.335–0.804) | 0.203 (0.086–0.479) | 0.001 | |
| Age (years) | 0.960 (0.929–0.992) | 0.935 (0.881–0.991) | 0.024 | 1.014 (0.981–1.049) | 0.965 (0.908–1.026) | 0.256 | |
| Sickle cell status | Negative | 1 | 1 | 1 | 1 | ||
| Positive | 1.434 (0.776–2.649) | 1.387 (0.736–2.615) | 0.312 | 0.780 (0.414–1.468) | 0.713 (0.365–1.396) | 0.324 | |
| Gravidity | 0.932 (0.825–1.053) | 1.046 (0.846–1.293) | 0.679 | 0.897 (0.793–1.014) | 0.748 (0.594–0.943) | 0.014 | |
| Parity | 0.905 (0.782–1.047) | 0.969 (0.755–1.243) | 0.804 | 0.957 (0.826–1.109) | 1.110 (0.847–1.454) | 0.451 | |
Discussion
This study explored the complex interplay between anaemia and glucose-6-phosphate dehydrogenase deficiency in pregnancy. The study examined anaemia at two stages: at registration (13 weeks) and at 36 weeks. Additionally, the study explored the potential implications of concurrent anaemia with glucose-6-phosphate dehydrogenase deficiency.
The results showed an increase in the prevalence of anaemia over the course of pregnancy. The mean haemoglobin concentration for pregnant women at 13 weeks was slightly higher than the WHO threshold for normal levels. However, at 36 weeks, the mean concentration was below the threshold and there was a 1.5-fold increase in the prevalence of anaemia between 13 and 36 weeks. Many factors, including biological and socioeconomic variables, have been linked with reduced haemoglobin levels. Haemoglobin concentration decreases during the mid-third trimester (Kalaivani, 2009) as a result of increased plasma volume, which leads to a decrease in blood viscosity (Peace and Banayan, 2021) to facilitate placental circulation (Tan and Tan, 2013). This may be a contributory factor to the decrease at 36 weeks seen in the present study.
Glucose-6-phosphate dehydrogenase deficiency was prevalent among pregnant women with anaemia, but the association was not statistically significant. The overall prevalence of the deficiency found in the present study was greater than the estimated prevalence among the general population, which is 7–19% in Ghana (Carter et al, 2011; Owusu-Agyei et al, 2012; Amoako et al, 2014; Owusu et al, 2015). At 13–36 weeks, the present study found a co-occurrence of glucose-6-phosphate dehydrogenase deficiency and an increased prevalence and severity of anaemia as pregnancy progressed. These findings are consistent with other studies, which have reported that glucose-6-phosphate dehydrogenase prevents oxidative damage to red blood cells. This defence mechanism is weakened by a deficit of the enzyme, potentially increasing the risk of red blood cell oxidation and anaemia (Gautam, 2016).
Women who were older were significantly less likely to be anaemic at 13 weeks but not at 36 weeks. Stephen et al (2018) reported that older mothers in northern Tanzania had higher haemoglobin concentrations than younger mothers. Studies in Ghana, Nigeria and India have likewise reported an increased risk of anaemia in younger pregnant women (Ahenkorah et al, 2016; Okoh et al, 2016; Sapre et al, 2018). As the majority of pregnant women at Cape Coast Metropolitan Hospital were less than 35 years old, it is important that haemoglobin concentration estimates are taken when these women attend antenatal care.
Gravidity was significantly associated with anaemia at 36 weeks but not at 13 weeks. Pregnancy and labour are known to impact anaemia (Astriana, 2017). The depletion of iron in the body during pregnancy means that a woman's risk of anaemia increases with the number of pregnancies and births she experiences (Astriana, 2017). This iron loss over the course of pregnancy could explain the marked difference between anaemia at 13 and 36 weeks' gestation.
Sociodemographic factors such as education and ethnicity were not found to significantly influence anaemia in the present study, while marital status and employment did impact the likelihood of anaemia at 13 and 36 weeks respectively. In Jimma, Ethiopia, Belachew and Legesse (2006) explored factors related to anaemia among pregnant women and reported that education and employment were both significantly linked with anaemia. In Dakar, Chowdhury et al (2015) found that anaemia was significantly associated with pregnant women's education. Specifically, pregnant women with higher education could benefit more from health education during clinic visits, translating into achieving adequate haemoglobin levels (Raru et al, 2022). The impact of sociodemographic factors may vary in local contexts as a result of differences in the social, economic and cultural demands on pregnant women. Physically demanding occupations such as trading, farming, fishing, artisanry and formal jobs can cause considerable stress to a pregnant woman's body. Women who are not working full time may have more time to practice self-care, reduce stress and physical exertion, access family and community support and have some flexibility with antenatal care appointments (Wong Shee et al, 2021; Corchero-Falcón et al, 2023; Felisian et al, 2023). It is known that women living with a partner generally have a better diet than single mothers (Farbu et al, 2014). This suggests that social support and partnership can influence nutritional decisions and overall dietary habits and outcomes. Other reports suggest that being single may allow women autonomy, reduce stress from toxic relationships and mean they do not need to care for children or partners, potentially leading to more flexible personal and health-seeking schedules (Chamie, 2019). These factors may enhance overall health and improve haemoglobin levels. However, the population size, study site and time period for the present study may have impacted the findings, as contrary findings suggest that unemployment directly affects income, nutrition, access to healthcare, stress, mental health issues, affordability of supplements, access to information and the general wellbeing of pregnant women (Gaillard et al, 2014; Bongomin et al, 2021).
Pregnancy-related anaemia poses significant risks to the health of both the mother and the fetus. Decreased oxygen delivery and increased exhaustion and risks of problems during labour and birth are all associated with anaemia (Noronha et al, 2012). Additionally, there is a greater chance of preterm birth, low birth weight and developmental problems for the fetus (Stephen et al, 2018). Unpublished district data show that the Cape Coast Metropolitan Hospital recorded 18, 13 and 11 stillbirths in 2020, 2021 and 2022, respectively. In addition, 53, 103 and 39 low birth weights were recorded in these years. Comorbid glucose-6-phosphate dehydrogenase deficiency and anaemia can worsen these risks, demanding more intensive antenatal care and monitoring (Engwa et al, 2017). In Ghanaian antenatal care units, the standard management and prevention of anaemia and glucose-6-phosphate dehydrogenase deficiency during pregnancy and among newborns include dietary management (iron folate, vitamin B and C supplementation), haemoglobin monitoring, hydration, genetic counselling and referral to tertiary care where necessary (Ghana Ministry of Health, 2017; WHO, 2018).
Implications for practice
Clinicians and midwives should exercise caution when determining pregnant women's anaemia status and the present of glucose-6-phosphate dehydrogenase deficiency, particularly in areas where deficiency is prevalent. Early detection could allow individualised treatment and management, including close monitoring of haemoglobin levels, use of iron supplements and control of anaemia-related problems.
Limitations
As this study was retrospective, the authors relied on available data and excluded records that did not meet the inclusion criteria. In Ghana, pregnant women are free to initiate and complete care where they wish, meaning that records for women who did not complete antenatal care at the hospital were excluded. Therefore, it is possible that associations between variables were missed as a result of these exclusions. However, the data obtained were sufficient for the analysis performed to make meaningful deductions. Future studies could adopt a prospective cohort design to minimise bias and limitations.
Conclusions
This study found a high prevalence of anaemia among pregnant women at 13 and 36 weeks in Ghana. Few women registered at the hospital for antenatal care were glucose-6-phosphate dehydrogenase deficient, and the majority of these women were anaemic at 36 weeks. Age, marital status, employment and gravidity were significantly associated with anaemia. These findings could be used to inform clinical practice, improve antenatal care and contribute to the broader discourse on maternal and fetal health. The authors suggest use of a comprehensive approach that includes consideration of genetic and nutritional factors to reduce the risk of anaemia in pregnant women with glucose-6-phosphate dehydrogenase deficiency and optimise outcomes for mothers and children.


