Expressing breast milk is an alternative to direct breastfeeding that can allow mothers greater flexibility in when and where babies are fed, while maintaining exclusive breastfeeding. When mothers return to work, expressing breast milk can allow for continued exclusive breastfeeding, at a time when it can be difficult to breastfeed directly (Rokom, 2011; Danso, 2014).
The Indonesian context
In Indonesia, mothers are allowed 3 months maternity leave, after which it is expected that they will return to work (Central Government Indonesia, 2003). While there are national standards (Ministry of Health, 2013) that support breastfeeding mothers and exclusive breastfeeding, few workplaces have policies that strictly enforce these standards. Additionally, the number of working women, and therefore the number of working mothers, may be increasing. In Manado, a city in Indonesia, data from the Central Statistics Agency (2018) show that the number of women in the workplace is increasing; the city had 11 260 working women in 2017 and 12 343 in 2018. This increase in the number of working women may impact exclusive breastfeeding.
In 2018, the rate of exclusive breastfeeding in the North Sulawesi province of Indonesia was 26.5%, in the bottom third for Indonesia (Ministry of Health, 2018). Although data show that the proportion of babies aged <6 months being exclusively breastfed increased to 36.2% in 2023 (Tim Percepatan Penurunan Stunting Provinsi Sulawesi Utara, 2024), this is still far from the target. Working mothers may find it difficult to exclusively breastfeed their babies because of time constraints and the limited availability of breastfeeding facilities in the workplace. This can lead mothers to switch to formula and cease exclusive breastfeeding (Rokom, 2011).
Barriers to exclusive breastfeeding
Several factors have a negative impact on exclusive breastfeeding and duration of breastfeeding, including returning to work, as well as a lack of knowledge, confidence and physical and psychological support from the environment, including the workplace (Khariena Akbar et al, 2022).
Studies have shown that working mothers can find it difficult to breastfeed, although there are strategies that ensure babies are still exclusively breastfed (Basrowi et al, 2015). Barriers to exclusive breastfeeding for working mothers may be intrapersonal or influenced by environmental factors (interpersonal, organisational or community). These barriers include a lack of confidence in breastfeeding, which can be influenced by misinformation and cultural elements, lack of support from healthcare workers and misperceptions in the workplace about breastfeeding management and lactation rooms (Agustina et al, 2020).
To address these barriers, mothers should be able to access information about exclusive breastfeeding and expressed breast milk management when returning to work. This information should be available from the start of pregnancy, and mothers should also be able to communicate with their workplace about their needs. Healthcare workers should educate mothers and their family about the benefits of exclusive breastfeeding, so mothers are supported to continue exclusive breastfeeding when they return to work (Agustina et al, 2020).
The impact of technology
Technological advances and the widespread use of smartphones and mobile software applications (apps) in healthcare delivery have had a significant impact on delivery models. Interactions with healthcare workers that were typically handled face to face are now increasingly complemented or supported by virtual meetings, including via mobile health apps (Saputra et al, 2023). Women who are pregnant or have recently given birth are likely to seek health information online. A study of first-time African-American mothers found that all participants used at least one mobile app during pregnancy or after giving birth (Asiodu et al, 2015). Researchers have recommended designing interactive professional breastfeeding apps to promote long-term breastfeeding behavior (Meedya et al, 2021).
According to Saraswati et al (2020), android apps are an easy-to-use medium for accessing health information, and can be used to increase knowledge, attitudes and skills related to health. A literature review by Surtania et al (2023) found that education through apps was more effective in improving mothers' knowledge, attitudes and skills than ordinary care. This may be because this information is easily accessible, without the requirement to book and attend an appointment with a healthcare professional. Apps may therefore be a useful tool in supporting mothers to maintain exclusive breastfeeding, by addressing barriers such as misconceptions and lack of knowledge, and improving knowledge, attitudes, skills and self confidence (Seyyedi et al, 2021). However, further tests are needed to explore the effect of smartphone-based education before and after birth (Seyyedi et al, 2021).
The ASIPku application is an innovative mobile app that aims to assist working mothers with exclusive breastfeeding. It provides health information about the importance of exclusive breastfeeding and expressed breast milk management, including how to express, store and give expressed breast milk. The app can also include a pumping schedule, and provide reminders to users to express breast milk. It contains scientific articles and videos related to breastfeeding, as well as testimonials from working mothers who have exclusively breastfed. The app provides direct consultation with breastfeeding counselors, as well as a group of working mothers, via WhatsApp.
Research aims and objectives
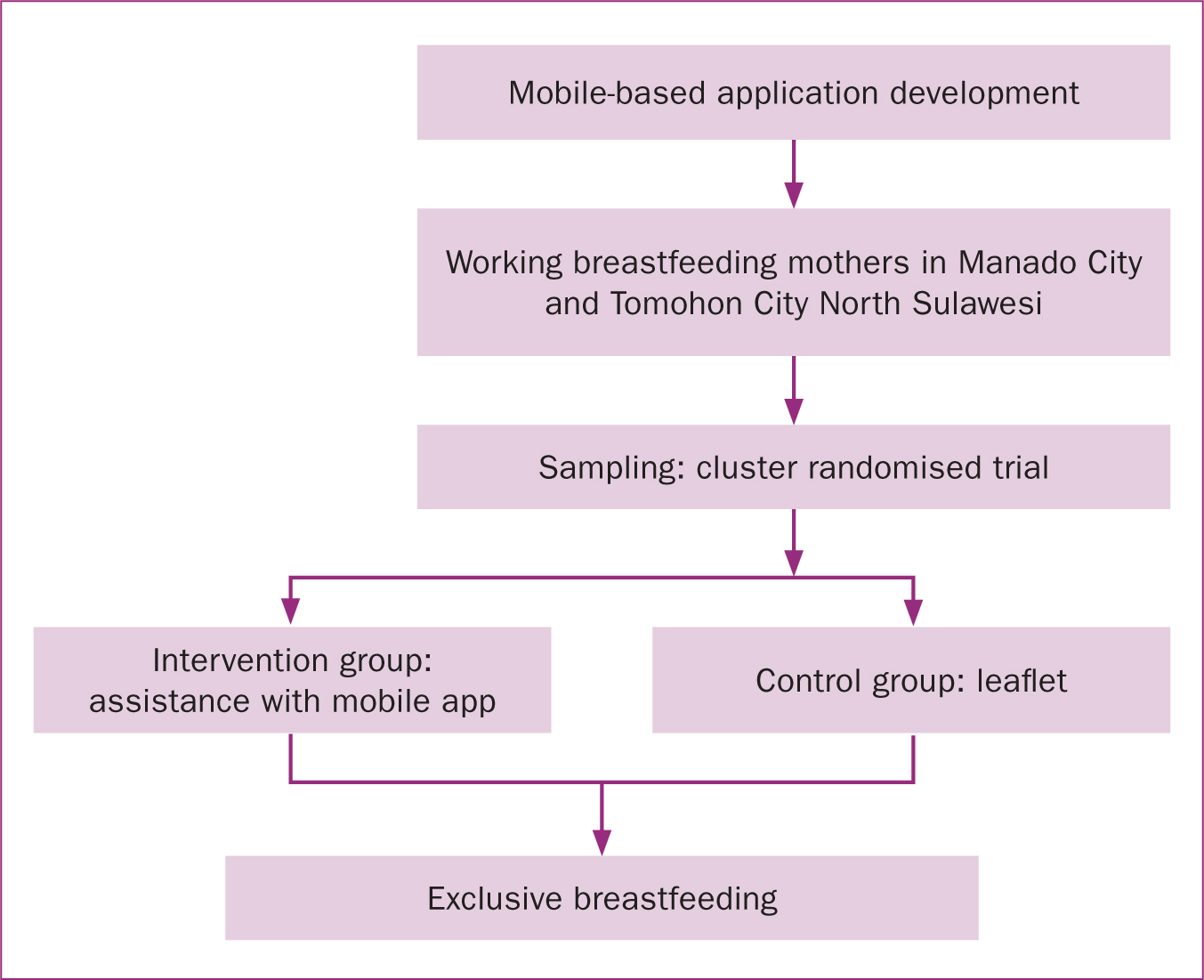
This is a follow-up study to a previous publication on using educational videos to educate pregnant women on expressed breast milk management (Sarimin et al, 2023). One year on from the first study, after participants had given birth, the present study was conducted to explore the impact of providing breastfeeding mentoring through the ASIPku mobile application among working mothers in North Sulawesi. Figure 1 outlines the complete research process. The aim was to increase the number of women who were exclusively breastfeeding in a working mother group by providing mentoring.
Methods
This quasi-experimental study was a randomised control group, using a pre-test, post-test design. The participants were women recruited while pregnant for the previous study, who had since given birth. The inclusion criteria for the previous study selected for working mothers.
Sampling
A total of 100 participants were included in the previous study and followed on to the present study, assigned previously to intervention (n=50) and control (n=50) groups. Cluster randomised sampling was used, where each sub-district in two cities, Tomohon and Manado, was sampled for participants using the Slovin formula. This was the second stage of research on assisting breastfeeding mothers, meaning the researchers had followed the participants since they were approximately 4 months pregnant.
Intervention
The intervention group received assistance through the ASIPku app, where information was provided in Bahasa. Participants were guided in use of the app via a Whatsapp group, and asked to use it over 6 months, after which data were collected. The videos and e-modules in the app were created and uploaded by the research team. The app included several article links as additional references, sourced from the websites of the Ministry of Health and Indonesian Breastfeeding Mothers Association. The information contained on the app is regularly monitored and kept up to date by the researchers. Users of the app were also able to directly contact counsellors on expressed breast milk, who were members of the research team.
The control group was minimally treated with a leaflet containing information on expressed breast milk management, created by the researchers for the purpose of this study.
Data collection
To measure exclusive breastfeeding, participants were given a questionnaire taken from a previous study, where answers were rated using a Guttman scale (Rahayu, 2015). Data were collected between June and July 2023, 6 months after women gave birth, by visiting them directly.
Data analysis
To ascertain the effect of the intervention on exclusive breastfeeding, Chi-squared tests were used with P<0.05 to establish significance.
Ethical considerations
This study was approved by the research ethics commission of the Health Polytechnic of the Health Ministry of Manado (reference: KEPK.01/05/100/2022). The study also received a research permit recommendation from the governments of Manado Regency through the National Unity and Politics Agency of North Sulawesi, Indonesia. Participants gave written informed consent to take part in the study.
Results
Table 1 outlines participants' sociodemographic characteristics. The majority of participants were 31–40 years old (53.0%), worked in the government sector (58.0%), were multiparous (55.0%), and had female children (52.0%).
Table 1. Sociodemographic characteristics
| Characteristic | Frequency, n=100 (%) | |
|---|---|---|
| Age (years) | ≤30 | 47 (47.0) |
| 31–40 | 53 (53.0) | |
| Occupation | Privately employed | 42 (42.0) |
| Government employee | 58 (58.0) | |
| Gravida | Nulipara | 45 (45.0) |
| Multiparous | 55 (55.0) | |
| Child's sex | Male | 48 (48.0) |
| Female | 52 (52.0) |
Table 2 shows the results of statistical testing for exclusive breastfeeding between groups. In the intervention group, 96.0% of participants were exclusively breastfeeding compared to 6.0% in the control group. The Chi-squared test showed that this difference was statistically significant(P=0.000). It was concluded that assistance via the ASIPku mobile application was effective in increasing the rate of exclusive breastfeeding among working mothers.
Table 2. Exclusive breastfeeding
| Exclusive breastfeeding | P value | ||
|---|---|---|---|
| Yes | No | ||
| Intervention (n=50) | 48 (96.0) | 2 (4.0) | <0.001 |
| Control (n=50) | 3 (6.0) | 47 (94.0) | |
Discussion
The purpose of this study was to explore the effect of support through the ASIPku application on exclusive breastfeeding among working mothers in North Sulawesi. The majority of the intervention group was exclusive breastfeeding at the point of data collection, whereas almost all women in the control group were not. Thus, the information obtained by the intervention group via the application is likely to have increased women's knowledge of expressed breast milk management. This has an impact on behaviour, making women more likely to continue exclusively breastfeeding for longer. This application is one example of the ways in which digital platforms can be used to provide education for breastfeeding mothers.
As technology evolves, digital platforms are becoming an important source of health information on a global scale. The COVID-19 pandemic drove rapid transformation of the healthcare system, especially in terms of the role of e-health and telemedicine (Tilahun et al, 2021). Video and app-based content are optimised for mobile devices. With apps, health education can be spread widely, especially with the development of mobile technology throughout the world (Rumsfeld et al, 2016). Developments in mobile messaging technology have enabled the dissemination of health messages on a large scale, and researchers are now increasingly realising the potential of mobile phones and tablets for improving health education interventions (Sondaal et al, 2016). As a result of the perceived need to access information directly through social networks and the internet, many people prefer apps and smartphones as their main mode of communication (Frazer et al, 2016). High-quality evidence-based apps and websites can be used by various populations to improve health outcomes (Skouteris et al, 2017; Harari et al, 2018; DeNicola et al, 2020).
Universal use of the internet and mobile devices has made digital media increasingly prevalent in delivering health information messages in communities and hospitals. Digital media can include discussion forums, websites, mobile applications and short message services. Information and support received digitally have the potential to reduce or shorten visits to hospitals or health services (Wulansari, 2017). Digitisation of health message delivery can overcome economic, distance and time barriers to accessing information (Schnitman et al, 2022).
The rapid and continuous growth of mobile health applications creates new opportunities to improve behaviour related to health and wellbeing. At the same time, it can raise concern about the quality of applications and the information that users receive. To enable long-term breastfeeding, mothers need education and support from early in pregnancy, continuing until after they give birth. Apps for breastfeeding mothers need to contain reliable information and be easily accessible for users (Meedya et al, 2017). Lupton (2017) highlighted the effectiveness of digital media for education on breastfeeding and the high rates of participant acceptance of this mode of education, reporting that 96% of participants in their intervention group were exclusively breastfeeding following education with a mobile app.
The authors' previous study (Sarimin et al, 2023) used a WhatsApp group to form a community of breastfeeding mothers. Providing support to this group was effective in increasing their confidence in providing exclusive breastfeeding. Support from healthcare professionals and other mothers was an important element of improving confidence. Mothers who have a community to share their breastfeeding experiences with, and find answers to to questions while breastfeeding, are likely to be empowered to continue exclusive breastfeeding for longer (Pasambo et al, 2022).
Mobile health interventions, including mobile apps, are highly effective in supporting exclusive breastfeeding practices among breastfeeding mothers. Acar and Şahin (2024) developed a mobile app-based breastfeeding program and evaluated its effectiveness. The authors reported that mothers who used the app showed a decrease in breastfeeding problems and an increase in exclusive breastfeeding. Rosa (2022) explored the use of an Android-based app for breastfeeding counselling and found that those receiving counselling were 3.3 times more likely to be exclusively breastfeeding than those in the control group. This systematic review found that 60% of mHealth interventions resulted in an increase in knowledge and behaviour changes in breastfeeding mothers (Rosa, 2022). Three studies have reported higher knowledge about breastfeeding among users of a mobile app, and that the education provided also influenced the duration of exclusive breastfeeding (Alnasser et al, 2018; Doan et al, 2020; Seyyedi et al, 2021). Research has also shown that methods to encourage and reinforce good behaviour related to breastfeeding include in-app prompts, regular breastfeeding schedule reminders and the use of theory-based content (Te Ku Nor et al, 2023).
In addition to support from healthcare professionals and that provided by health education and apps, a mother's workplace is an important factor in determining mothers' ability to provide exclusive breastfeeding. A systematic review by Vilar-Compte et al (2021) found that workplace interventions increased the duration of breastfeeding and prevented early introduction of formula milk. Interventions include providing a lactation room, rest time to express breast milk and organisational policies. These interventions are important to ensure that working mothers receive protection and support in providing exclusive breastfeeding. Yeşildere Sağlam et al (2023) developed assessment criteria to evaluate support for breastfeeding mothers in the workplace. They highlighted that providing support for breastfeeding mothers in the workplace improves the health status of mothers, babies and the community, having a positive impact on the economy by reducing health service costs. To achieve a fair working environment for women who breastfeed, support and attention is needed on all three ecological levels, individual, interpersonal and organisational.
Implications for practice
A number of studies have shown that mobile apps are an effective method for providing exclusive breastfeeding support for breastfeeding mothers. In the future, apps should be developed based on the latest theories, following the development of best practices including stakeholder involvement.
The present study's results have implications for increasing promotion of exclusive breastfeeding; the use of an app is likely to make it easier for users to access information and connect breastfeeding mothers with the community and breastfeeding counsellors.
Limitations
The sample for this study was taken from only two cities in North Sulawesi Province. It is recommended to expand this research to reflect the experiences of breastfeeding mothers more widely.
Conclusions
Mobile apps are an effective way to deliver health education and support to women. By providing information on expressing breast milk, these apps can be used to support women who are pregnant and those who have given birth. This is likely to improve women's knowledge of expressing breast milk, which will improve rates of exclusive breastfeeding among working mothers, by making it more accessible to this group.
Key points
- Returning to work can make it difficult for women to continue exclusively breastfeeding babies.
- Barriers to exclusive breastfeeding for working mothers include lack of confidence in breastfeeding, influenced by misinformation, lack of support from healthcare professionals and misperceptions in the workplace about breast milk management and lactation rooms.
- Breastfeeding mothers may benefit from information about exclusive breastfeeding and expressed breast milk management when returning to work.
- The rapid advancement of technology and the widespread use of smartphones and mobile software applications provides an opportunity for healthcare professionals to incorporate technology into traditional care.
- This study explored the use of a mobile app to provide digital mentoring on expressed breast milk to working mothers with babies, finding that the app was an effective way to deliver health education and support.
CPD reflective questions
- How could digital mentoring be used to support working breastfeeding mothers in your own practice?
- What challenges might you face when using digital technologies to provide breastfeeding education and support?
- How do the practical implications of this study's findings support the development of future digital mentoring programmes?


