Despite recommendations from the World Health Organization (WHO) that the ideal rate for caesarean sections (CS) should be between 10 and 15%, the CS rate in the UK has not reduced in recent years and remains at 25% (Health and Social Care Information Centre, 2015; WHO, 2015), with Nottingham University Hospitals NHS Trust's rate comparable at 24%. As the main provider of postnatal care, the midwife is responsible for delivering wound care to these women. This care comprises both action and advice to prevent surgical site infections (SSI) and care within professional boundaries in the event of a SSI occurring. SSI is a risk with any surgical procedure, although the risk is acknowledged to be greater with certain procedures, such as vascular and cardiac surgery (Reilly et al, 2006). CS has typically been viewed to be a low-risk procedure due to the younger age and perceived good health status of patients. However, due to health-care advances, many women are now having children who would previously have been unable to due to pre-existing conditions (Anderson et al, 2013; McGiveron, 2015). The altering health status of the pregnant population requires us to reconsider the importance of wound care and the risk of SSI in this group.
There is no national reporting mechanism for CS SSI, so rates are unknown. Wloch et al (2012) report a rate of 9.6% in England, although only 36% of patients were contacted. Work undertaken in Ireland in 2011 identified a rate of 16%, with 93% of patients included in the study (Enohumah et al, 2011). In Norway, rates of 21% have been reported (Dyrkorn et al, 2012). Similarly in Brazil, where the current CS rate is above 50% (Ramires de Jesus et al, 2015), a CS SSI rate of 23% has been reported (Cardoso del Monte and Pinto Neto, 2010). A local surveillance programme identified a Trust CS SSI rate of 26% (Berry, 2012, unpublished). Public Health England, who administer the national SSI reporting programme for other procedures on behalf of the Government, have recently piloted a CS SSI surveillance programme, suggesting CS SSI is being recognised as an issue that requires investigation (Wloch et al, 2012).
CS SSIs can have a significant impact on a woman's physical and psychological health and may also affect her ability to care for, and bond with, her baby (Boyle, 2001). Developing a wound infection may lead to more serious, complicated conditions, such as sepsis—the leading cause of maternal death according to the last Confidential Enquiries into Maternal Deaths report (Cantwell et al, 2011). CS SSIs have the potential to have a significant impact on maternity services and create a substantial burden on NHS funding and resources across acute and primary care.
As lead for the surveillance programme, the author observed that midwives' knowledge of wound care may be lacking. These observations took the form of patient discussions, reviews of patient's notes and discussions with midwives and suggested education on wound care was a need in midwifery. With the recent publication of the Francis report (2013), the importance of having staff with the right knowledge, skills and experience to deliver high quality care has been highlighted.
In order to develop an education package that addressed the learning needs of midwives, a knowledge-assessment needed to be carried out to identify gaps in existing knowledge. This would ensure the package addressed the learning needs of users. DeSilets (2006) stresses the importance of capturing the learner's views when planning knowledge-assessments. A mix of audience and expert participation in identifying the priorities for knowledge-assessments was also discussed by Jazwiec (1991). It is vital that midwives' views are sought at the earliest opportunity to promote engagement and effectiveness with the knowledge-assessment and subsequent education. This will ensure the knowledge-assessment captures midwives' needs and is not based on the assumptions of the author or educator. This is supported by DeSilets (2007) who warns against relying on the suppositions of those developing such tools.
Nobbs and Crozier (2011) acknowledge that CS wound education is a need. However, a literature search found no research that sought practising midwives' views on the subject. While Boyle (2001) concludes by stating good wound care should be part of every midwife's role, there is no evidence as to whether this is the case in current practice. Similarly, Nobbs and Crozier (2011) further state that training is needed to improve midwives' knowledge of wound care and advise that maternity units should undertake evaluations of knowledge and deliver training in this area, but do not propose or discuss how any of this may be achieved. Similarly, national guidelines are concerned with wider issues such as reducing the CS rate (National Institute for Health and Care Excellence (NICE), 2013) or obstetric issues such as surgical technique or antibiotic prophylaxis (NICE, 2011), but not with postnatal wound care. There are no specific wound care guidelines for maternity, and no mention of CS wound care in the Trust's general guidelines.
Aim
The aim of the research was to investigate midwives' views of their knowledge and the need for education in relation to CS wound care, prior to devising a knowledge assessment.
Ethics
The project was reviewed by the Trust's Research and Innovation department and was deemed to be service evaluation. The project was registered as per the relevant Trust policy.
Methods
Tool
A questionnaire survey was chosen as the data collection method. This method was chosen as it would allow a large sample size to be evaluated within the time frame for data collection, which was 4 weeks, and would provide the quantitative data needed to inform subsequent work in this area. The areas of focus were:
As the aim of the survey was to consult midwives to inform a knowledge-assessment, no questions were included that tested knowledge against guidelines and policies.
The majority of questions were closed questions as there were only a certain number of possible responses. Two open-ended questions were provided for detailed responses. Five-point Likert scales were used to determine midwives' perception of their agreement or disagreement with various statements. Content validity was checked by considering each question in turn and asking if it would generate the information required in a usable format. Face validity was conducted with representatives from the target population. The questionnaires were piloted with seven participants and appropriate changes made. The majority of comments related to clarification of questions or statements.
Sample
The survey aimed to assess the opinions of the practising midwives employed by the Trust working within hospital and community settings. Convenience sampling was used to access the amount of midwives required. Due to time constraints, the aim was to sample 10% of the target population. The Trust employs 440 midwives across the hospital and community setting, resulting in a target of 44 participants.
Data collection
The questionnaire was distributed to midwives attending two clinical study days. Participants would use 30 minute break periods to complete the questionnaire, allowing them adequate time to complete the questionnaire. To achieve the required numbers of respondents, staff were also approached in clinical areas and asked to participate. The clinical areas included were two labour suites and four inpatient wards across two sites. Participants who had been involved in the pilot phase were excluded.
IBM SPSS Statistical Version 21 was used for data entry and analysis. Based on the data and the number of participants, only descriptive statistics were generated.
Results
Fourty-four questionnaires were completed by midwives of bands 5-7.
Need for education
The majority of participants (74%, 32/43—one participant did not respond) reported having had no previous education in relation to CS wound care, similarly 61% (27/44) reported they did not have enough knowledge to manage a CS wound appropriately. Eighty-four percent (37/44) of participants agreed or strongly agreed with the statement ‘I feel I would benefit from education’ (Figure 1).
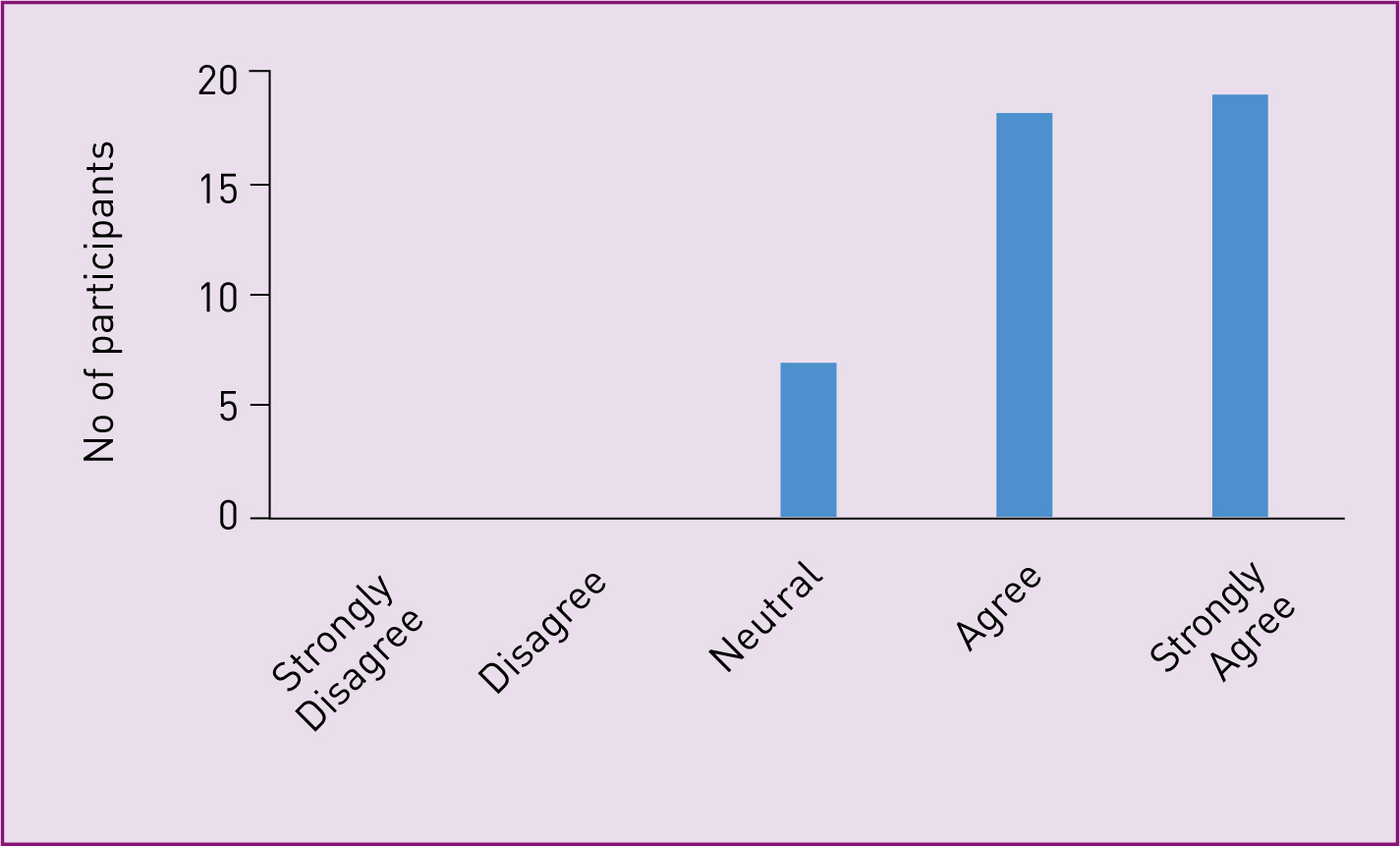
This quantitative data was supported by qualitative comments from participants:
‘Midwives muddling along not knowing what they are doing.’
‘Education needs most apparent.’
‘Not enough midwives have sufficient knowledge … resulting in women not receiving optimum care.’
Education content
Participants were asked to indicate which topics they felt should be included in a training package and asked to indicate any topics not listed (Table 1). Wound dressings and wound assessment were the most popular topics for inclusion.
| Topic | Number of responses (participants could tick more than one response) |
|---|---|
| Dressings | 36 |
| Wound assessment | 34 |
| Treatment of infected wounds | 31 |
| Patient advice | 29 |
| Aseptic technique | 13 |
Education delivery method
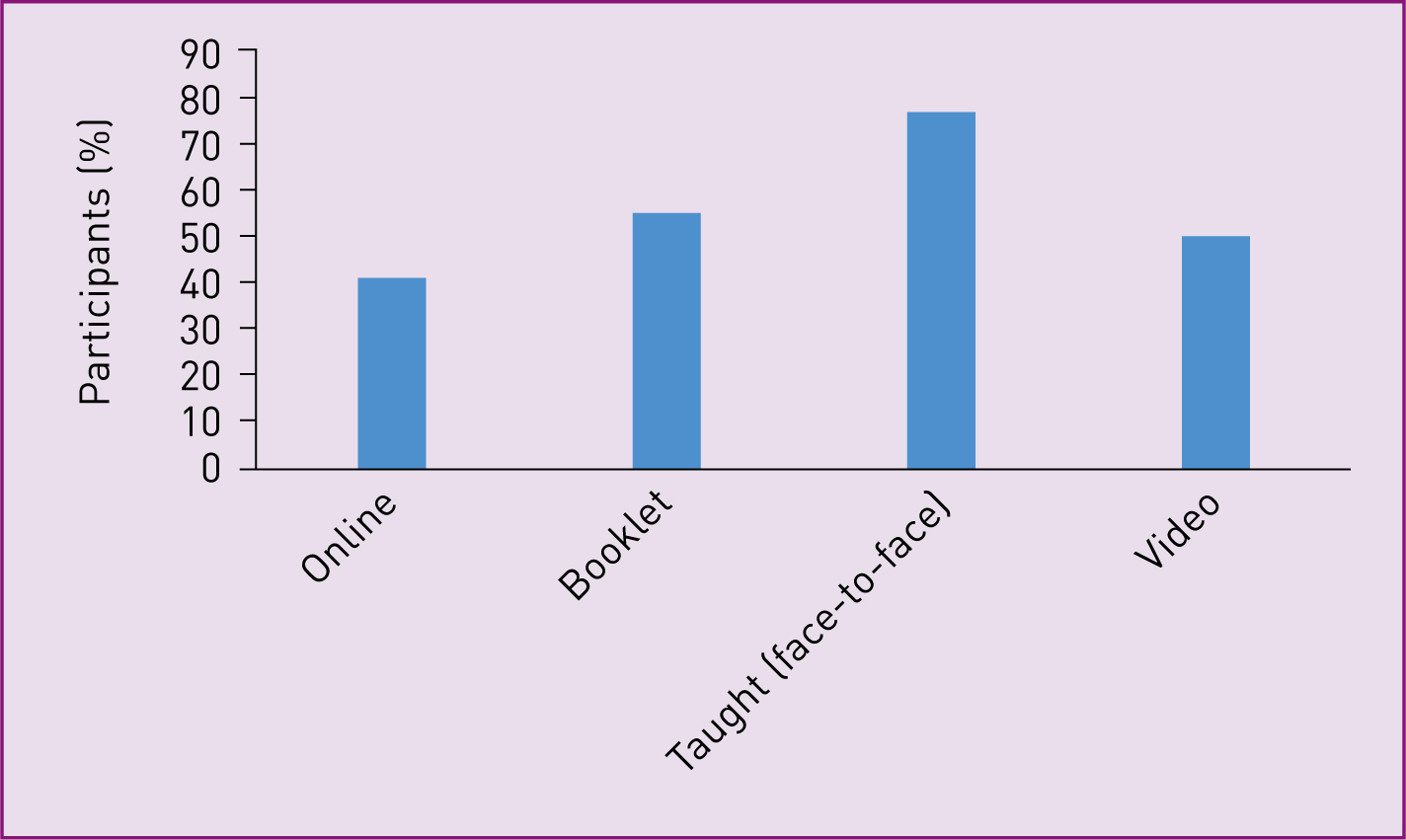
Participants were asked to indicate their preferred delivery method for wound care training. The options were: online, booklet, face-to-face or video format. Participants rated each method from 1 (least preferred) to 5 (most preferred). Figure 2 shows the percentage of participants who rated each method as a 4 or 5.
Discussion
Data from this study suggest that midwives' in this Trust feel there is a clear need to deliver education around CS wound management to ensure that women who have had a CS are appropriately cared for. These data support the available literature (Nobbs and Crozier, 2011) and echo the sentiments of the Francis (2013) report, which also emphasised the importance of ensuring staff have appropriate knowledge. Many of the recommendations in the Francis report relate to the behaviours, competencies and skills required of all staff to deliver high quality care. Qualitative comments from the participants in this study suggest that maternity staff feel ill-equipped to effectively manage a CS SSI. In order to provide a safe and effective care environment for women, these potential short-falls in knowledge and confidence must be addressed.
While two of the papers reviewed advocate staff training on CS wound care (Boyle, 2001; Nobbs and Crozier, 2011), neither suggest nor discuss what should be included in training. This is the first study to determine information from midwives about their perceived areas of knowledge deficit. As such, this information will influence a knowledge-assessment, focusing on areas of need for the target population. As midwives have identified the specific areas they require education on, engagement is likely to be higher as the content is relevant to them and not generic. This is supported by DeSilets (2006) and Jazwiec (1991). In the absence of this engagement, the learner is not recognised as having valuable contributions to make to the process and elements participants see as vital may be missing. Interestingly, aseptic technique, which is a key feature in most wound care education was not rated as a topic for inclusion. This may be due to staff feeling confident with this aspect of wound care, or seeing other areas as a priority.
Regarding how midwives want education to be delivered, a taught session was rated as the most useful method of delivery. The three other suggested methods received similar responses in terms of their usefulness. Each method of delivery offers advantage and disadvantages. While taught sessions were the most popular with staff and do allow for interaction and discussion, there are practical issues with location, equipment, recruiting staff to present and ensuring good attendance, in addition to the complications of providing a taught session for 440 staff around a 24-hour clinical service. There are also cost implications, not only in terms of venue but also in staff time for presenters and those attending (Brunero and Lamont, 2010; Preston et al, 2012).
While staff may perceive a taught session to be most useful, Williams et al (2001) compared knowledge and skills between those who attended a lecture and those who completed an on-line package. The students perceived they had learned more from the lecture than online, but those who used the on-line package had greater skills acquisition when measured objectively. Numerous other articles state the benefits of online learning. O'Neill et al (2011) revealed a significant improvement in health-care-associated infection knowledge among medical students after completing an online e-learning programme and the majority of students were positive about the learning experience. Desai et al (2000) reported similar results when they evaluated an interactive computer-based learning package. Brunero and Lamont (2010) utilised scenario-based learning shared via e-learning to improve nurse's knowledge and skills concerning patient relationships. They reported an increase in knowledge and suggest e-learning as a viable resource for nursing teams.
Online packages can be easily updated and after the initial outlay for design are free to access. They also offer the advantage of being accessible repeatedly at any time, which contributes to the regular reinforcement needed to embed knowledge. Additionally, Lymn et al (2008) found students felt access to online reusable learning tools increased their confidence within the topic area. Online packages also offer shared learning between specialities, organisations and countries. However, perceived issues with online learning include ICT implications, such as access to computers, log-on details and compatibility issues. Health-care workers also have concerns that if they are seen at a computer, it will be interpreted negatively by patients and visitors. However, this can be addressed by better use of existing IT facilities and protected time away from clinical areas which can be better incorporated into clinical services.
As highlighted in the 2015 Nursing and Midwifery Council's (NMC) Code of Practice, midwives are required to practise in line with the best available evidence (section 6) and to recognise and work within the limits of their competence (section 13) (NMC, 2015). Education is essential in allowing midwives to fulfil these requirements.
Limitations
Of the clinical areas visited, the two labour wards produced the highest number of participants. This may be due to the nature of the clinical areas with ward staff frequently not having time to participate in the project. While staff working on the labour suite could be core, or rotational staff, and will all have some exposure to CS wound care, the permanent ward staff will be able to provide the most accurate information on CS wound care. It was this group where there was lowest engagement, which may have had an impact on the quality of data received.
This work was conducted at one large teaching hospital split across two sites. While a representative sample of 10% was obtained, a larger sample may have resulted in different responses. Performing this work at another hospital may identify similar or different issues.
The response rate has not been recorded for this piece of work. Significant numbers of staff were approached to participate and declined due to time pressures in the clinical area. All of the participants approached on the study days completed questionnaires. In future, the response rate would be recorded. Various study days and staff forums take place throughout the year so had time not been a limiting factor, these settings would have been the location for all questionnaires to be completed.
Conclusion
This is the first time midwives' views have been sought regarding the need for CS wound care education. The findings of this work concur with the few published papers concluding there is a need for CS wound care education within midwifery from a midwives' perspective. This work adds to the literature with topics midwives feel should be the focus of such education and useful methods of delivering it. The outcomes of this work can be used to inform a knowledge assessment capable of identifying midwives learning needs, to inform the content of the education package.

