Scotland has historically seen low rates of breastfeeding and the Scottish Government has identified breastfeeding initiation and maintenance as a public health priority (Scottish Government, 2018). In support of these goals, NHS Boards within Scotland have implemented the UNICEF Baby Friendly Initiative by revising policies and increasing training for midwives and health visitors to support breastfeeding (Broadfoot et al, 2005). Initiation rates have increased but maintenance remains a problem. The Scottish Government's Diet and Healthy Weight Delivery Plan sets out a commitment to reduce drop-off in breastfeeding rates at 6–8 weeks after birth by 10% by 2025 (Scottish Government, 2018). Of babies born in 2017–2018, breastfeeding was initiated in 64% of cases but at the 6–8 week follow-up, just 41% continued to receive any breastmilk (ISD, 2018). Despite its substantial commitment to breastfeeding, high rates of breastfeeding drop-off remain a stubborn problem in Scotland.
The majority of drop-off occurs in the first two-weeks postpartum (ISD, 2018). The Infant Feeding Survey estimates that 86% of mothers who have given up breastfeeding would have liked to have continued breastfeeding for longer (McAndrew et al, 2012). These findings suggest a role for helping pregnant women plan for breastfeeding.
Planning cards have previously been used in interventions among patients to promote adherence to HIV medications (Goujard et al, 2003). Here we test whether an obstacles/tips card can help women adhere to their breastfeeding intentions. The card details the most frequent problems identified by mothers attempting to develop a breastfeeding routine. This in itself might reassure new mothers that their experiences are not unusual and so enhance mothers' feelings of self-efficacy, which would be expected to reduce drop-off (Blyth et al, 2002; Brockway et al, 2017). Additionally, the card gives actionable tips on structures that can be put in place prior to the birth that will facilitate breastfeeding.
We also test an enhanced planning card, which asks the woman to write on the card how many weeks/months she intends breastfeeding. Importantly, the response to this prompt is private; the authors never saw what the participant answered. The literature suggests that prompting people to articulate their intentions can affect attention and memory processes that are relevant to acting on those intentions (Sheeran and Orbell, 2000). Prompts of this nature have been shown to promote other health behaviours eg attendance at medical testing (Sheeran and Orbell, 2000) and dietary change (Rothman et al, 2009).
Development of the card
The card was designed with three goals in mind: maximising relevance to mothers; deliver ing state-of-the-art, evidence-based guidance; and communicating in user-friendly terms. To maximise relevance to mothers, we consulted the literature to identify which problems mothers identify as inhibiting breastfeeding.
We began by looking to the most recent quantitative data from the UK to answer this question, the UK Infant Feeding Survey (McAndrew et al, 2012). It reported the following as the most frequently cited reasons: baby not sucking/rejecting the breast (33% of cases), having painful breasts or nipples (22% of cases), and the mother feeling she had insufficient milk (17% of cases). These data come from the UK as a whole, whereas our population of interest is Scotland. We cross-referenced these data with reasons reported in recent qualitative surveys of mothers from the Scottish population (Hoddinot, 2012; McInnes et al, 2013). These Scottish studies confir med ‘breastfeeding is uncomfortable or painful’ and ‘I don't think I have enough milk’ as the first two problems we listed on the card. Items 3 and 4 were informed by the result from the Infant Feeding Survey that 23% of mothers who breastfed for less than one week had reported that it would be helpful to get more support from family and friends (McAndrew et al, 2012). Mothers living in Scotland reported that one motivation for quitting breastfeeding was to give their significant other an opportunity to bond with the baby and that an aid in continuing breastfeeding was having support in forming routines (McInnes et al, 2013). The final card is presented in Figure 1.
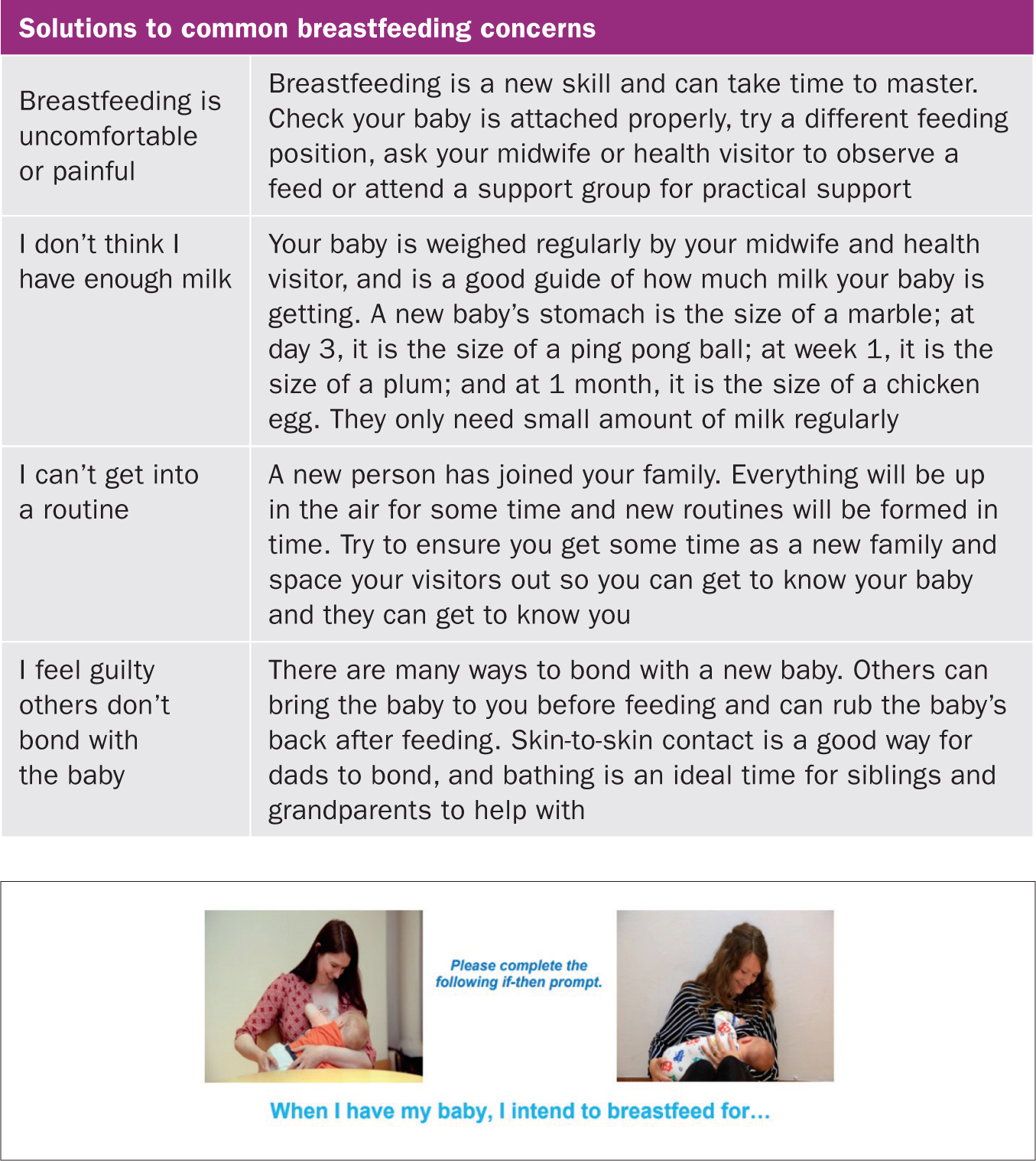 Figure 1. (including the table). The obstacles/tips card (top) and intentions prompt (bottom)
Figure 1. (including the table). The obstacles/tips card (top) and intentions prompt (bottom)
Suggested solutions were taken from the UNICEF website, the NHS.UK website and the Scottish Government parent support website, Parentclub. The language of the recommendations posted on these websites was adapted to fit the card. For instance, the Parentclub website posts the following advice: ‘It's a skill that you and baby need to learn … There's nothing more natural or healthier for you and your baby, but equally nothing can really prepare you for it. So don't be too hard on yourself, and remember to just take it one feed at a time, step by step. And if you have any difficulties or you're worried about anything, you're not alone-just talk to your midwife or health visitor as soon as possible, and they'll help you’ (2018). For the card, we summarised this as, ‘Breastfeeding is a new skill and can take time to master. Check your baby is attached properly, try a different feeding position, ask your midwife or health visitor to observe a feed or attend a support group for practical support’.
We sought feedback on the appropriateness of the messages, the wordings and the design of the cards from participants at a mother-and-baby group in Lothian. We also asked this group whether the card would have been helpful to them when they were starting breastfeeding. There was consensus that the content of the card was relevant and that it presented the information clearly and in plain English. No mother answered that she would have found receiving the card to be unhelpful or upsetting.
The pilot test
Participants
In June 2018, 81 pregnant women were recruited. We posted an announcement that a study was seeking pregnant women who were more than 36 weeks pregnant and who intended breastfeeding. Of the participants, 20 were recruited via webforums in the Edinburgh area: Mumsnet, Netmums, Edinburgh for the under fives and Edinburgh Gossip Girls. The remaining participants were recruited at antenatal classes in yoga and relaxation in the Edinburgh area.
Procedures
One author [TMG] announced during antenatal classes that we were recruiting pregnant women for a study and invited those who intended breastfeeding and were over 36 weeks pregnant to stay after class. After class, volunteers were handed the informed consent documents. The systematic allocation to condition took place as follows. Informed consent documents were alternated in advance so that every third document had attached a standard obstacles/tips card; another third had attached the enhanced obstacles/tips card with the prompt on its rear-side; the final third had no card attached.
TMG then invited the women to read thoroughly the documents and to reply with their contact number for follow up, their due date and, if applicable, to fill in the prompt on the reverse side of the card.
Participants recruited online were sent emails with the informed consent as an attachment. It was alternated whether those emails included as an attachment the standard obstacles/tips card; the enhanced obstacles/tips card or no additional attachment. For both the online and antenatal groups, it was made explicit that the women would never be asked to show us what they had written on their cards.
We followed up by text message 10–14 days after the due date that the pregnant woman had specified on her informed consent document. The message asked, ‘can you let me know how you are feeding your baby today. Please reply, breastfeeding, formula feeding or mixed feeding. If you have changed feeding method since you gave birth, can you let me know what feeding method you were using on discharge from hospital?’ Women who did not reply were resent the message after 24 hours. The study was approved by the General University Ethics Panel in May 2018. As this is a pilot test, we did not conduct a power analysis.
Analyses
We conducted binary logistic regressions on whether mothers were breastfeeding and whether they were exclusively breastfeeding using STATA 12.1. We report two-tailed p-values.
Results
Table 1 presents summary statistics of participants in each condition. Out of our sample, 4 of 81 (5%) did not respond to our text messages, so we have follow-up breastfeeding data from 77 mothers. Due dates spanned 19 days (ranging from 15 June 2018 to 2 July 2018) and were coded as a continuous variable from 1–19.
Table 1. Summary statistics by condition
| Control (n=28)n (%) | Obstacles/tips card (n=26) n (%) | p-value vs control | Enhanced obstacles/tips (n=27) n (%) | p-value vs control | |
|---|---|---|---|---|---|
| Independent of treatment (n=81) | |||||
| Mother has other children n (%) | 18 (64%) | 16 (62%) | 0.835 | 15 (56%) | 0.509 |
| Age | 31 | 32 | 0.218 | 33 | 0.184 |
| Number of other children | 1.2 | 0.84 | 0.369 | 0.72 | 0.316 |
| Due date | 10.0 | 8.1 | 0.164 | 8.8 | 0.381 |
| Recruited at antenatal class n (%) | 20 (75%) | 20 (77%) | 0.869 | 21 (74%) | 0.937 |
| Potentially impacted by treatment (n=77 for breastfeeding outcomes) | |||||
| Sample attrition n (%) | 3 (11%) | 0 (0%) | n/a | 1 (4%) | 0.338 |
| Any breastfeeding at discharge | 20 (80%) | 23 (88%) | 0.131 | 22 (85%) | 0.224 |
| Exclusive breastfeeding at discharge | 16 (64%) | 18 (69%) | 0.360 | 21 (81%) | 0.056 |
| Outcome variables, collected 10-14 days post-due date (n=77) | |||||
| Any breastfeeding n (%) | 16 (64%) | 22 (85%) | 0.033 | 22 (85%) | 0.027 |
| Exclusive breastfeeding n (%) | 13 (52%) | 18 (69%) | 0.094 | 21 (81%) | 0.009 |
There was no characteristic that varied significantly across condition, though sample attrition approached statistical significance: whereas all women in the standard obstacles/tips card condition replied to the follow-up text message, three women in the control condition did not (n=54, x2=2.95, p=0.086).
Figure 2 depicts feeding method by condition at each point in time. The lower panels of Table 1 report these same data alongside the p-values returned from univariate logistic regressions. There were no reliable differences in rates of breastfeeding on discharge from hospital. At follow-up, women in both card conditions were reliably more likely than mothers in the control condition to be engaging in any breastfeeding (standard card: p=0.033; enhanced card: p=0.027). Relative to the control group, mothers in the enhanced card condition were more likely to be engaged in exclusive breastfeeding (p=0.009).
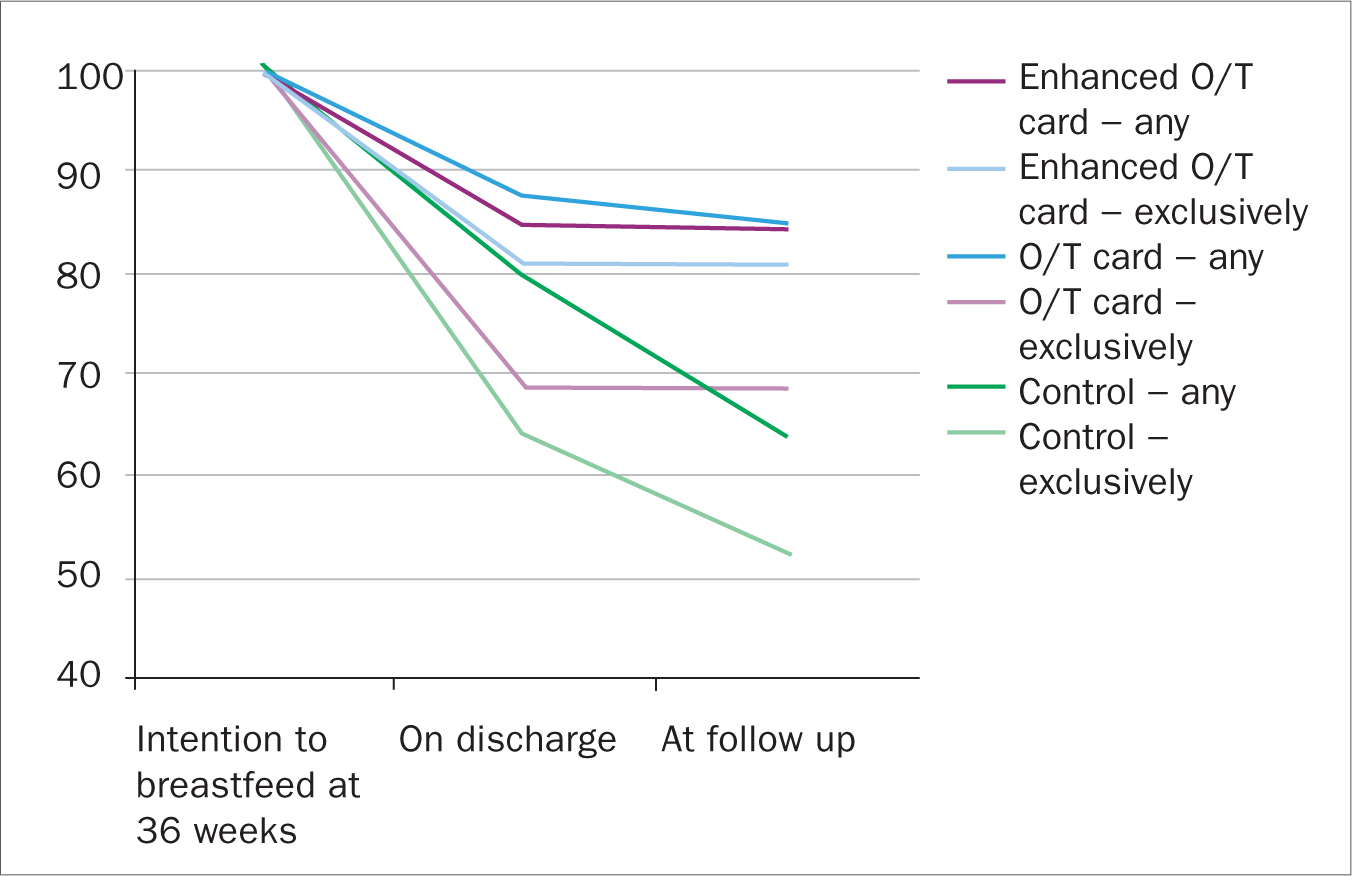 Figure 2. Percentage women engaging in any breastfeeding and exclusive breastfeeding at each timepoint, by condition
Figure 2. Percentage women engaging in any breastfeeding and exclusive breastfeeding at each timepoint, by condition
Multivariate analyses
Table 2 reports the results of a binary logistic regressions on feeding outcomes that control for mother's characteristics. Model 1 estimates predictors of the infant receiving any breastmilk at 10–14 day follow-up. It shows that infants whose mothers received either the standard obstacles/tips card or the enhanced obstacles/tips card were significantly more likely than those in the control group to receive any breastmilk at follow-up.
Table 2. Results of multivariate logistic regressions of breastfeeding
| Model 1Any breastfeeding at 10−14 days post due date | Model 2Exclusive breastfeeding at 10−14 days post due date | Model 3Drop-off from breastfeeding between due date and 10−14 days post due date | ||||
|---|---|---|---|---|---|---|
| Factor | Odds-ratio (95% CI) | P-value | Odds-ratio (95% CI) | P-value | Odds-ratio (95% CI) | P-value |
| Obstacles/tips card | 5.677 (1.24–26.08) | 0.026 | 2.681 (0.78–9.21) | 0.117 | 0.137 (.002−0.97) | 0.047 |
| Enhanced obstacles/tips card | 9.413 (1.68–52.72) | 0.011 | 6.865 (1.63–28.91) | 0.009 | 0.066 (0.01−0.75) | 0.028 |
| Mother's age | 0.877 (0.77–1.00) | 0.046 | 1.004 (.90–1.11) | 0.943 | 1.135 (0.96–1.34) | 0.136 |
| Any other children | 1.547 (0.21–11.58) | 0.671 | 0.985 (0.18–5.49) | 0.987 | 1.424 (0.12–16.6) | 0.778 |
| Number of other children | 1.563(.56–4.37) | 0.395 | 1.597 (0.63–4.03) | 0.322 | 0.647 (0.21 – 2.01) | 0.452 |
| Due date | 1.071 (0.94–1.22) | 0.307 | 1.063 (0.95–1.19) | 0.286 | 0.875 (0.72–1.06) | 0.167 |
| Recruited at class | 0.989 (0.21–4.69) | 0.989 | 1.095 (0.29–4.09) | 0.893 | 1.877 (0.16–21.85) | 0.615 |
| Constant | 24.757 (0.32–1927.8) | 0.149 | 0.296 (0.01–11.71) | 0.516 | 0.015 (0.16–21.85) | 0.165 |
Model 2 reports the results of a binary logistic regression on the infant being exclusively breastfed at follow-up. It shows infants whose mothers received the enhanced obstacles/tips card were significantly more likely to be exclusively breastfed than those in the control group at follow-up (p=0.009). Exclusive breastfeeding in the standard obstacles/tips card condition was not significantly higher relative to the control condition (p=0.117), nor was it significantly lower relative to the enhanced card condition (p=0.195).
Model 3 reports the results of a binary logistic regression on drop-off. Drop-off is coded as a binary variable that indicates that a mother was breastfeeding on discharge from hospital and was not engaging in any breastfeeding at follow-up. Drop-off was significantly reduced relative to the control condition by both the standard obstacles/tips card and the enhanced obstacles/tips card.
Discussion
To summarise, pregnant women who were presented with a simple card describing obstacles/tips were significantly more likely to be breastfeeding at follow-up than a comparable group of women who received no card.
We speculate that the mechanism through which the card has its effects is by promoting breastfeeding self-efficacy (Blyth et al, 2002). To the extent that breastfeeding is natural, new mothers may expect it to come naturally ie effortlessly and without complications. That expectation could lead mothers to conclude that any difficulties they experience mark them out as exceptional. The card informs mothers that it is normal to experience some difficulties breastfeeding and so reassures that there is nothing ‘wrong’ with them or their baby. Additionally, the card provides actionable tips and these may have given mothers a sense of increased control over the breastfeeding process. Future research might investigate whether breastfeeding self-efficacy mediates the effect on breastfeeding outcomes.
There are limitations to our study that should be addressed in a follow-up on a larger sample. First, feeding method data should be based on actual date of birth whereas here it was based on due date. Our method introduced a source of noise because the same due date can be shared by babies born up to four weeks apart. This source of noise is insuperable in these data—we do not have data on when the woman actually gave birth. Second, measures of breastfeeding behaviour are self-reports and so may suffer from measurement error and self-presentation bias. This is a weakness that our study shares with administrative data—the Scottish NHS also records breastfeeding data using mothers' self-reports (ISD, 2018). Future research would more precisely measure the magnitude of the card's effect by collecting follow up data in a manner that removes these sources of noise.
A further limitation of the current research concerns recruitment. All participants who were recruited at antenatal classes will have learnt that some participants received a card and that some received a card that asked them how long they intended breastfeeding. It is possible that this led some participants who were not assigned a card to answer the prompting question for themselves; in effect, it might be that some participants who we coded as being in the control condition were in fact treated with the prompt. If this spillover occurred, then breastfeeding rates among our control group might have been inflated. This would mean that the difference in outcomes across the treatment and control groups would have been underestimated relative to what would be observed in a blinded study.
A cleaner estimate of the causal effect of the card would be obtained if women were unaware that there existed other study conditions eg if the card were presented to women during the course of a one-to-one consultation with a midwife. A further advantage of trialling the card as part of standard antenatal care is that doing so might deliver a more representative sample. We recruited a convenience sample of women from antenatal yoga classes and online forums. The women who engage these services during pregnancy might have different characteristics than does the general population of pregnant women. This might explain why our control group had higher rates of breastfeeding than the Scottish average: 64% of mothers in our control group were engaging in any breastfeeding at 10–14 days postpartum versus 51% in Scotland as a whole (ISD, 2018).
Conclusion
These data suggest that presenting women in late stage pregnancy with planning cards might reduce drop-off from breastfeeding and increase exclusive breastfeeding at 10–14 days postpartum. The card requires few resources to deliver effectively and so we consider it worth investigating its potential in a randomised controlled trial on a larger and more representative sample. Ideally, that study would also investigate the feasibility of delivering the cards as part of standard antenatal practice eg during the 36-week midwifery appointment.
Key points
- Many women stop breastfeeding sooner than they would have liked
- A planning card that prepares pregnant women to deal with breastfeeding obstacles could reduce drop-off
- An experiment tested the effect of giving the obstacles/tips card to pregnant women
- Rates of breastfeeding drop-off among mothers presented with the obstacles/tips card were four-fold smaller than among a control group of mothers who were randomly selected not to receive the card
CPD reflective questions
- At what stage of their pregnancy did women receive the obstacles/tips card?
- How did the authors decide which obstacles to highlight on the obstacles/tips card?
- How might the obstacles/tips card improve breastfeeding self-efficacy?


