Evidence-based standards are an important means for ensuring safe and effective care for birthing women (World Health Organization, 2021). The provision of one-to-one care for women in labour is one such standard. Research shows that one-to-one care in labour is associated with better outcomes and higher levels of satisfaction for mothers (Hodnett et al, 2012; National Institute for Health and Care Excellence (NICE), 2014; Bohren et al, 2017; Sosa et al, 2018; Bjerga et al, 2019; Buerengen et al, 2022). However, the provision of one-to-one care is difficult to provide and measure. It is difficult to find and retain the number of staff required to offer such care (Harrington et al, 2020). Additionally, lacking a tool to measure staffing levels in relation to the acuity level of those being cared for makes it impossible to know how many staff are needed (NICE, 2015).
In the Netherlands, there has been a national standard for birth care since 2016 (College of Perinatal Care (CPZ), 2016). This standard states that birthing women should be provided with one-to-one care for active labour and the immediate postpartum period (CPZ, 2016). This was reaffirmed in 2020 (CPZ, 2020), and in 2021, the Dutch National Health Care Institute (2023) mandated compliance with the standard of birth care for all providers of maternity services in the Netherlands.
While there is a system for the audit of perinatal statistics in the Netherlands (Perined, 2023), there is no nationally accepted system for audit of staffing in relation to service provision. In addition, there is no nationally agreed evidence-based guidance relating to minimum staffing levels in hospital midwifery service provision. Consequently, since its inception in 2016, there has been no national assessment of compliance with this element of the birth standard, largely because there is no agreed upon tool in use to facilitate this aim.
Reliable tools for measuring staffing levels in birth-care settings do exist (Royal College of Midwives, 2018) and there are many examples of best practice in relation to staffing issues (Clarke and Dondaldson, 2008; NICE, 2015). While a full explanation of the Dutch model of maternity service provision is not within the scope of this article (see Cronie et al, 2012 for a fuller description), it is important to understand that although most midwives in the Netherlands are employed in primary care, and most women begin labour with their primary care midwife, most births occur in hospitals accompanied by a different healthcare team (Perined, 2020). However, lacking an audit tool, little is known about the provision of one-to-one care during labour (Cronie et al, 2012; Perined, 2020). At a minimum, all birthing women in the Netherlands should receive care according to the national standard, and some women will require more intensive care.
When staffing issues are not documented and prioritised, dramatic consequences ensue (Kirkup, 2022; Ockenden, 2022). Poor staffing is commonly cited as a primary factor in the chain of events leading to significant harm to mothers and babies. However, having a standard without a way to measure its attainment means it is not possible to estimate, with any degree of certainty, how (or even if) the standard is being met. This, in turn, limits proper planning, implementation and evaluation of care.
A systematic review by Cronie et al (2022) identified Birthrate Plus (Ball et al, 2003) as the most widely used midwifery-specific tool, which gives the insight needed to model midwifery numbers, skill mix and deployment and to inform decision making about safe and sustainable services. However, it is not known if Birthrate Plus methodology can be applied to the Netherlands context. This pilot study was designed to test the suitability of the Birthrate Plus tool for use in Dutch hospital maternity settings, with the goal of future audit.
Methods
Birthrate Plus has been validated as a patient acuity measurement tool in the UK (Royal College of Midwives, 2018). To assess its value in a different setting, and to measure staffing levels, a pilot study using Birthrate Plus in the Netherlands was designed. Recognising that the time required to observe and evaluate levels of care on a maternity unit was prohibitive, the Birthrate Plus tool was used to compare actual full time equivalents on a unit with the full time equivalents needed to offer one-to-one care according to the level of acuity of women in labour.
Sampling
There are 71 hospitals with midwifery departments in the Netherlands. A purposive sample of 10% (n=7) of these hospitals was selected. In order to test the use of Birthrate Plus in a broad spectrum of hospital settings in the Netherlands, the following selection criteria were applied: a minimum of one teaching and one non-teaching hospital, a mix of hospitals from urban and rural areas, as well as at least one tertiary-level, university hospital. Two authors (DJC and AR) used their network of midwifery and gynaecology contacts to randomly recruit the sample.
Data collection
In discussion with the developers and owners of Birthright Plus, it was decided that collection of sufficient data would require a minimum period of 4 months in each hospital. Since Birthrate Plus uses birth and non-birth related attendance to calculate total labour ward activity, the goal was to capture all episodes of labour ward attendance in this 4-month period in each of the hospitals. Since a random spread of labour ward activity was desirable, data collection was spread over 12 months from November 2021 to November 2022.
Each hospital was asked to supply an Excel spreadsheet containing an anonymised dataset of attendance characteristics for each patient attending the labour ward over 6 months (to allow for missing or incomplete data). The attendance characteristics in the dataset were:
- Reason for attendance
- Length of attendance
- Gravidity/parity
- Gestation (if pregnant)
- Length of labour
- Intravenous access during attendance
- Use (and type) of analgesia during labour
- Whether continuous fetal monitoring was used during attendance
- Single/multiple pregnancy
- Presence of additional medical problems necessitating consultant oversight
- Method of birth
- Trauma/type to perineum following birth
- Apgar score at 5 minutes
- Birth weight of the baby
- (Presence of) congenital abnormality
- Livebirth/stillbirth/neonatal death
- Intravenous continued after birth
- Blood transfusion
- Emergency spinal/general anaesthetic
- Admission to intensive care setting.
Where calculations were expressed for an annual basis, the sample data were adjusted accordingly. To protect their identity, hospitals in the pilot study were randomly labelled A through E. The case mix data was used to build a picture of the number and type births for each hospital during the study period. Using the tool, births were coded in terms of their complexity from category 1 (low) to category 5 (high), according to the characteristics of the birth.
Definition of terms
The Birthrate Plus tool works on the principle that all birthing women will receive one-to-one care. For the purposes of this study, one-to-care was calculated as beginning with the active-phase of labour, including (but not limited to) the commencement of continuous fetal monitoring, or confirmation of the active phase of labour, or the period where continuous attendance of the obstetric caregiver is advisable and ending 2 hours after the birth is completed. As specified in the Dutch standard, one-to-one care in the hospital setting must be delivered by a specialist obstetric caregiver, defined as a midwife/clinical midwife (registered midwife working in a hospital setting), a physician-assistant clinical midwife (a registered midwife with an additional qualification) or a doctor (which includes a general practitioner with specific experience in midwifery, an obstetric resident or an obstetrician) (Dutch Organisation of Obstetricians and Gynaecologists, 2012; Royal Dutch Organisation of Midwives, 2015; CPZ, 2020).
A full-time equivalent was defined as 36 hours per week. Annualised hour calculations were expressed using the standard uplift calculation (for holidays/sickness and study leave) of 19%, in accordance with the National Dutch collective labour agreement for hospitals (Netherlands Federation of Hospitals, 2023). This meant that the actual total (annual) hours for one full time equivalent was 1516 hours.
Data analysis
One researcher (DJC) collated and analysed data. To assess the reliability of coding, a test of inter-observer variability was performed, where a second researcher (AR) analysed a random, anonymised selection of data using the Birthrate Plus tool. A Kappa coefficient test was then performed to check the level of variance between the two researchers. The kappa coefficient (k=0.7) shows a substantial level of agreement between coders.
The time needed for a category 1 birth served as the baseline for calculating the workload ratio of births in the other four categories. In the UK, the time allotted for a category 1 birth is 8 hours. To adjust for the Dutch setting, Wiegers and Janssen's (2005) research was used; they calculated that the time required for an uncomplicated birth was 6 hours. As the complexity of care increases, the caregiver hours for that patient population increases, as complex cases require additional time for indirect care of the woman, her baby and partner, administration, liaising with other midwifery or medical colleagues and completing all necessary paperwork.
Using the Birthrate Plus methodology, category 1 and 2 births were assessed at 100% of their actual time, category 3 at 120%, category 4 at 130% and category 5 at 140%. The product was then compared to the baseline of 6 hours (category 1) to provide a workload ratio. For example, if a hospital's average length of labour for a category 5 birth is 10 hours, the workload ratio would be 10 hours multiplied by 1.4, then divided by 6 hours is 2.3, meaning the time needed for a category 5 birth is 2.3 times greater than a category 1 birth.
The total workload ratio was multiplied by the daily number of cases, to give a total workload index, which is the total workload generated from the number and case mix of births from each hospital. This can be used to calculate the caregiver hours required per day, which can then be upscaled per week/month. The actual hours analysis and workload ratios for each hospital are available from the authors on reasonable request.
The Birthrate Plus algorithm adds a 15% variance for unpredictability of workload and a further 5% to allow for time spent on administrative tasks. This is divided by 36 (the full time equivalent hours for hospital staff in the Netherlands). To complete the calculation, an additional 19% is added, which is the nationally agreed uplift for holidays/sickness and study leave.
To give a fuller understanding of the labour ward workload, the non-birth workload was also assessed and added to the calculation. The non-birth related workload consisted of an additional four workload categories: attendance of women who are not in labour and are sent home (category X), attendance of women who need some form of treatment but who are not in labour (category A), readmissions following birth (category R), other remaining non-birth activity (such as transfers), categorised as: ‘other’. Because of the small sample size, the standardised mean hours-per-case length of time for non-birth activity was used, as suggested in the Birthrate Plus algorithm. These data are available from the authors on reasonable request.
It is important to note that these calculations were based on, and limited to, an estimation of birth and non-birth activity during the study period in the hospitals included. The study is intended to give insight into the feasibility of using the Birthrate Plus tool for maternity service provision in hospitals in the Netherlands. To complete a more comprehensive assessment of the total workload of Dutch maternity service provision in hospital settings, the full range of patient care provided (such as antenatal and postnatal care and clinics) must be added to the workload indices. This aspect of data collection (while possible using the Birthrate Plus tool) was not within the scope of this study.
Ethical considerations
Ethics committee approval for the pilot study was granted in October 2021 by the research ethics committee at the coordinating site (reference number: ACWO 21u.310). Data collection involved retrospective collation and analysis of anonymised birth characteristics. As such, the committee judged the study to be outside the scope of the rules for Medical Research Involving Human Subjects Act (Central Commission on Non-Human Research, 2022).
A full explanation of how the Birthrate Plus tool works is available in Ball and Washbrook (1996). Permission was gained from the owners of the Birthrate Plus tool to use the case-mix and hours-analysis elements of the tool.
Results
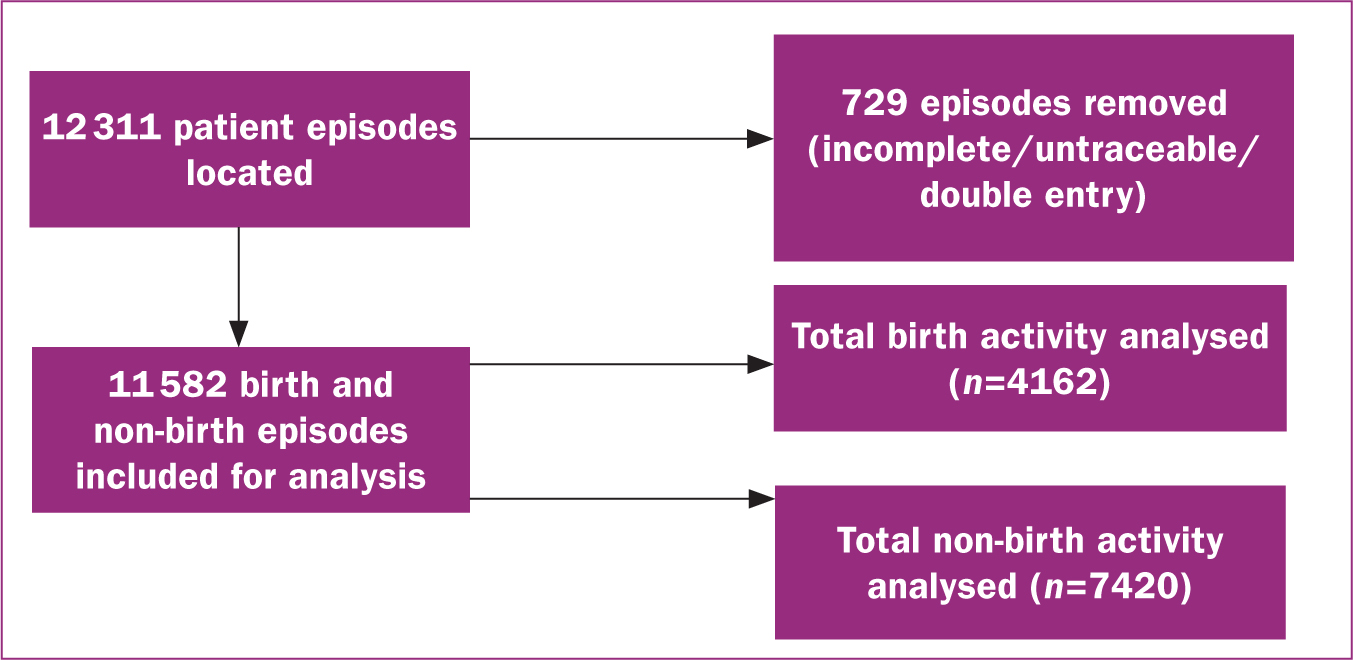
A total of 12 311 patient episodes were analysed from the five hospitals. Figure 1 shows a flowchart of the data used.
Case mix data
Analysis of birth activity found that 60% occurred in the higher case mix categories, 4 and 5. Although percentages varied, in all sites, most births were in category 4 and 5. The actual case mix of the birth data is shown in Table 1.
Table 1. Total actual case-mix birthrate categories analysed during study period
| Birthrate categories | Total | |||||
|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||
| % case mix | 21 | 1 | 18 | 40 | 20 | 100 |
| Total cases | 867 | 54 | 704 | 1811 | 726 | 4162 |
Skill mix and staffing patterns
Hospitals were asked to provide the usual pattern of skill mix for the labour ward area for the time period of data collection. Considerable variation was found in the skill mix across the sites. Although all worked with the same types of staff (clinical midwives, doctors, nurses and maternity care assistants), the proportion of each group making up the skill mix varied from site to site. Similarly, there was no commonality in the staffing ratios in terms of how many full time equivalents were employed.
Models of care differed between the sites, which affected how women were cared for. Models ranged from traditional settings with antenatal/postnatal and labour ward areas to family-centred care models where women were admitted to (and stay in) the same area for the duration of their stay. Skill mix, staffing ratios and models of care were heterogeneous across the sites. Data on the case mix, hours-analysis, workload ratio and non-birth activity for each of the hospitals studied are available from the authors on reasonable request.
Few births were found in category 2. The length of time for category 3 births ranged from 3–14 hours with an overall mean of 8.6 hours. The mean per hospital varied little from the overall mean (range of means 8.1–8.9). For category 4 births, the hours ranged from 3–19 hours with an overall mean of 10.2 hours, and the mean per hospital varied between 9.6 and 10.5 hours. For category 5 births, the range was 4–28 hours with an overall mean of 12.4 hours (range of means was 11.5–12.8 hours). Table 2 shows the averages for categories by hospital.
Table 2. Hours analysis: mean hours per category
| Category | Hospital | Range | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| 1* | ||||||
| 2† | ||||||
| 3 | 8.9 | 8.8 | 8.8 | 8.1 | 8.5 | 3–14 |
| 4 | 10.0 | 10.5 | 9.6 | 10.5 | 10.5 | 3–19 |
| 5 | 11.5 | 12.2 | 12.7 | 12.5 | 12.8 | 4–28 |
Births under-represented, analysed as equal to baseline
Workload ratio
The workload ratio is the multiplier used to calculate how much more work births from a higher category create (than those from a lower category) by using the time needed for a category 1 birth as a baseline. The mean workload ratio for category 3 births was 1.7 (range: 1.6–1.8). For category 4 births, the mean workload ratio was 2.2 (range: 2.1–2.3) and for category 5 births, the mean workload ratio was 2.9 (range: 2.7–3.0). Table 3 shows the workload ratios per category by hospital.
Table 3. Workload ratios
| Category | Hospital | Mean ratio | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| 3 | 1.8 | 1.7 | 1.8 | 1.6 | 1.7 | 1.7 |
| 4 | 2.2 | 2.3 | 2.1 | 2.3 | 2.3 | 2.2 |
| 5 | 2.7 | 2.9 | 3.0 | 2.9 | 3.0 | 2.9 |
Workload index
The workload index illustrates how many caregiver hours are needed per day in order to fulfil the standard for one-to-one care. The mean total workload index was 15 (range: 12.3–19.8). Table 4 shows workload indices by category and hospital.
Table 4. Workload index
| Category | Hospital | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| 1 | 0.8 | 0.5 | 1.3 | 4.0 | 0.9 |
| 2 | 0.0 | 0.1 | 0.2 | 0.3 | 0.1 |
| 3 | 1.5 | 2.4 | 1.5 | 3.4 | 1.9 |
| 4 | 8.4 | 5.4 | 5.8 | 8.6 | 7.6 |
| 5 | 3.5 | 4.0 | 5.4 | 3.5 | 4.1 |
| Total | 14.2 | 12.3 | 14.0 | 19.8 | 14.6 |
Assessment of workforce planning.
The total number of full time equivalent staff required for labour ward birth and non-birth activity ranged from 22.3–48.4 full time equivalents. Table 5 shows workforce planning calculations. The last two rows of Table 5 show the discrepancy between actual full time equivalents and those required to provide one-to-one care, based only on birth and non-birth activity during the study period, for each of the hospitals.
Table 5. Workforce planning
| Activity | Hospital | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Total caregiver hours per day | 82.0 | 74.0 | 84.1 | 119.0 | 87.3 |
| Total caregiver hours per week | 574.1 | 518.3 | 588.4 | 833.0 | 611.1 |
| Additional 15% workload variance | 660.3 | 586.0 | 677.0 | 958.0 | 702.8 |
| Additional 5% administration time | 693.3 | 626.0 | 711.0 | 1006.0 | 738.0 |
| Divide by hours per full time equivalent (36 hours) | 19.3 | 17.4 | 20.0 | 28.0 | 20.5 |
| Additional 19% uplift | 23.0 | 20.7 | 23.8 | 33.3 | 24.4 |
| Plus non-birth activity full time equivalent | 6.6 | 1.6 | 6.9 | 15.1 | 7.06 |
| Total full time equivalent required (birth + non-birth activity) | 29.6 | 22.3 | 30.7 | 48.4 | 31.5 |
| Current actual obstetric caregiver full time equivalent (birth + non-birth activity) | 15.4 | 9.6 | 16.3 | 17.3 | 13.4 |
Discussion
This study shows that Birthrate Plus can be used as an audit tool in the Dutch hospital maternity care setting. Although the desired sample size was not reached (a sample of 10% of hospitals was intended, but only 7% (n=5) were included), nonetheless, the analysis of more than 12 000 episodes of maternity care, from different types of hospitals over the course of 1 year, demonstrates the feasibility of using the electronic patient record systems in the Netherlands to populate the Birthrate Plus tool, allowing the evaluation of maternity care services.
There was consistency of measurement both within and among the hospitals studied. Most births managed in hospitals were categorised in the more labour-intensive, higher risk categories of four and five. This was consistent during the whole period studied and occurred across all hospitals. This is not surprising, as the majority of uncomplicated births in the Netherlands occur either at home, in birth centers or in clinical settings separate from obstetric departments (Perined, 2020). With regard to case-load mix, the present study's findings are not dissimilar to those from hospitals in the UK where Birthrate Plus has been used over a longer period (Shrewsbury and Telford Hospital NHS Trust, 2017; Care Quality Commission, 2018). Additionally, there were no significant differences in either the mean hours-per nor mean workload ratios for births in the higher categories (3–5) across all hospitals.
This study offers the first national audit of full time equivalents in place for providing care during labour in maternity care units in the Netherlands. More importantly, it shows that the hospitals in the sample had too few full time equivalents to offer one-to-one care, as required by the national standard for birth care since 2016 (CPZ, 2016; 2020; National Health Care Institute, 2023). The Dutch national standard for birth care is unequivocal; ‘women with a medical indication to birth in hospital should be from the moment of admission continuously supervised by a specialised caregiver’ (CPZ, 2016). Under Dutch law, the only care professionals licensed to give this care are doctors or midwives (Overheid.nl, 2022).
This study compared the actual staffing profiles for obstetric caregivers in the labour wards of the sample (full time equivalents for birth and non-birth activity) with the number of full time equivalents needed to provide one-to-one care, as calculated by Birthrate Plus. There was a shortfall of obstetric care providers ranging between 47% (best hospital) and 64% (worst hospital). These findings are in line with other studies that suggest that the Birthrate Plus tool can be used to assess the safety and quality of care (Ball et al, 2003; 2014; Yao et al, 2016; Altaweli et al, 2020). In the UK and Australia, use of Birthrate Plus to assess safe staffing levels is mandated and more data have been analysed. In these cases, Birthrate Plus has been in use for longer and is used to predict how many staff are needed to provide one-to-one care (NICE, 2015; New South Wales Government, 2022). However, other studies suggest that not only is it important to have the correct numbers of staff but also to ensure that they have the correct skillset and are available at the right place in the right time (Sandall et al, 2017).
Strengths and limitations
This study is the first to examine staffing levels in the maternity wards of hospitals in the Netherlands, using a validated tool developed for this purpose. However, there are limitations that should be noted. Given the nature of the pilot study (a small sample of hospitals with varied patterns of skill mix and staffing provisions), as well as the lack of any evidence-based, national guidance documents specifying staffing ratios, it is difficult to accurately assess the full time equivalents required for one-to-one care.
This study shows that the Birthrate Plus tool can reliably capture the data necessary to assess workload, but the lack of pre-existing data meant that it was necessary to rely on standardised calculations based on UK data for some aspects of non-birth rated workload. This may mean that the calculations for these aspects are not truly representative of the actual workload in the hospitals studied. A larger sample is needed to calculate baseline norms in different case-mixes, an important element in the analysis of full time equivalents for clinical care of women birthing in the Dutch hospital maternity care setting. Further and better examination of the workload in more hospitals over a longer period of time is required to better answer this conundrum.
Conclusions
This study is the first to systematically examine workload in relation to the Dutch birth care standard of one-to-one care for birthing women. This pilot study reported a mismatch between actual full time equivalents and those needed to meet Dutch standard. This points to the need for further research relating to all aspects of service provision in the Netherlands, gathered over a longer period and from a larger variety of hospitals with differing models of care.
Key points
- Birthrate Plus can be used in the Netherlands for the purposes of audit and workforce planning in hospital maternity service provision.
- Using the Birthrate Plus tool, most births managed in hospitals were categorised in the more labour-intensive, higher risk categories (4 and 5).
- Hospitals surveyed during the pilot study had too few full time equivalents to be able to offer one-to-one care for birthing women.
CPD reflective questions
- What is workforce planning and why is it important for midwives?
- Why is it important that safe staffing levels in maternity service provision are met?
- What are evidenced-based standards of care and why are they important?
- What is one-to-one care in midwifery service provision and why is it important?
- What are audit standards in midwifery service provision and why are they important?


