Public health has long been recognised as a significant role in midwifery practice; most recently clearly articulated in the standards of proficiency for midwives and the education standards for midwifery education (Nursing and Midwifery Council (NMC), 2019a, b). Throughout history it has been recognised that mothers have a significant influence on family health; therefore, the public health role of the midwife in providing woman-centred care can have a significant impact on family and population health.
The Solihull Approach Antenatal Foundation Training provides a framework for promoting infant, maternal, family and population health through professional interactions during pregnancy. This health promotion may continue with the transfer of care to a health visitor, contributing to the ethos of continuity of care in the interdisciplinary team.
All midwives in Northern Ireland are provided with Solihull Approach Antenatal Foundation Training and encouraged to consolidate the approach into their clinical practice (Bassett, 2018). In addition, the Solihull Approach is embedded in group based antenatal care and education (‘getting ready for baby’) sessions developed as part of the Early Intervention Transformation Programme.
The Solihull Approach
The Solihull Approach was originally developed by Dr Hazel Douglas in the late 1990s and is a psychotherapeutic and behavioural model that initially emerged from observed health visiting practice. The antenatal resource pack was first published in 2010, with the most recent edition published in 2017 (Douglas, 2018). However, a multi-user subscription (period of 5 years) now provides easy access to all four of the latest versions of the Solihull Approach resource packs (antenatal, first five years, school years, fostering and adoption).
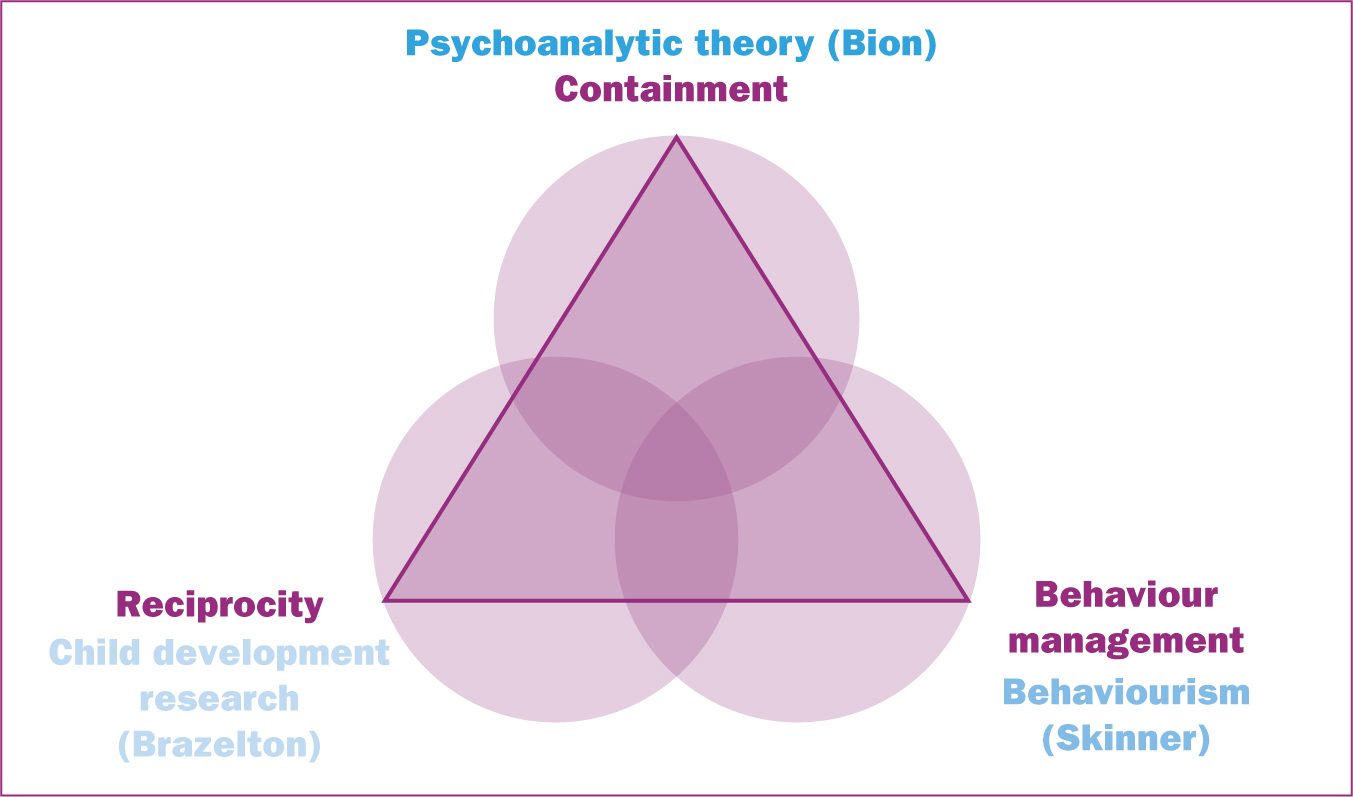
The Solihull Approach has the overarching aim to increase emotional health and wellbeing in the population and consists of three concepts. These concepts are embedded in psychological theories applied via a framework, which is underpinned by the principles of Bandura's (1977) social learning theory (Harris-Waller et al, 2019). The first of these concepts, containment, arises from psychoanalytical theory and was first described by Bion in the 1950s. Bion (2018) suggested that as human beings, we learn to process our emotions through interaction with one another and continue to do this from infancy and throughout our lives. In so doing, we learn how emotions can be both accepted and managed (Bion, 2018). It is a process by which an individual who listens to and is empathetic to another's distress, and without feeling personal distress, can ‘contain’ the other's emotional state. This feeling of containment can then enable the other to think more clearly for themselves. The concept aligns physical containment with emotional containment and views the maternal–fetus relationship as the first example of this. Containment can be seen not only in the relationship between parent and child, but is also emulated in the relationship between parent and practitioner, and professional relationships in the practice environment. Containment facilitates achievement of the second concept: reciprocity (Thelwell et al, 2017).
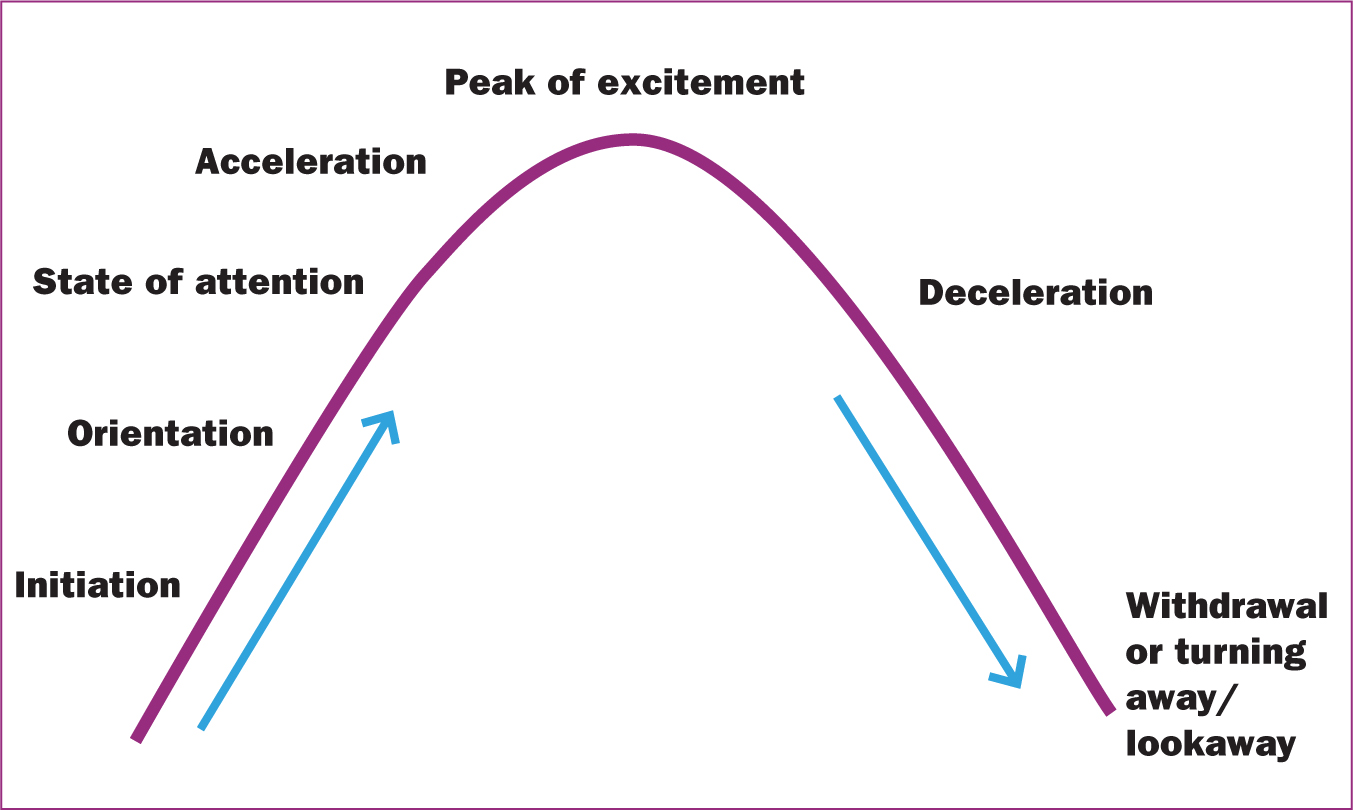
The concept of reciprocity evolved from child development research and was first described by a paediatrician, Dr Berry Brazelton (Brazelton et al, 1974). His research demonstrated that babies are socially active from birth, and observations of mothers' interactions with their babies demonstrated that there was a rhythm to these interactions. Further research developed the ‘dance of reciprocity’ and the specific steps in this rhythm of interaction between mother and child. The specific steps involve initiation, orientation, state of attention, acceleration, peak of excitement, deceleration and withdrawal or turning away (Douglas, 2018) (Figure 1). Reciprocity describes the sophisticated interaction between a baby and parent where both are involved in the initiation, regulation and termination of the interaction. The concept of reciprocity is not limited to the mother/parent–child relationship but can also be applied to all forms of relationships both personal and professional (Tan et al, 2017; Thelwell et al, 2017).
Containment and reciprocity subsequently lead to sensitive, customised behaviour change (Tan et al, 2017). Behaviour management forms the third concept of the model and is one that most health professionals will be familiar with, having been associated with operant conditioning theory originally proposed by Skinner (1938). Integration of these three concepts in one model facilitates a better understanding of the developing relationships in the mother–baby dyad and promotes emotional and mental wellbeing in families (Douglas, 2018) (Figure 2).
Containment and reciprocity are very relevant to midwifery practice and underpin the quality of attachment for parents and their newborn infant. Research has demonstrated that Solihull Approach antenatal groups have resulted in increased feelings of attachment in mothers and fathers and have decreased feelings of anxiety in relation to pregnancy, labour and birth (Douglas, 2016; Fagan et al, 2016).
Solihull Approach Antenatal Foundation Training is a 2-day programme aimed at facilitating understanding of the underpinning theories and how these are applied in practice. It includes opportunity for participants to discuss and demonstrate application of the approach to practice. Solihull Approach training has been facilitated for registered midwives as continuing professional development; however, there was a recommendation from the Northern Ireland Public Health Agency (personal communication, 17 November 2017) to incorporate it into undergraduate midwifery education. Queen's University Belfast is the sole provider of pre-registration midwifery education in Northern Ireland and currently provides two programmes: a 3-year BSc Midwifery programme (direct entry) and a 2-year MSc Midwifery postgraduate programme.
The Queen's University Belfast pre-registration midwifery curricula included components of the Solihull Approach in response to developments in clinical practice. However, there was no agreement or direction about how and when this should or could be integrated in the curriculum. This was further complicated by the range in timing of students' exposure to the Solihull Approach during clinical placements. Thus, the optimum timing varied depending on the student's practice learning environment and involvement in parent education. Furthermore, it was recognised that the Solihull Approach has the potential to be beneficial to midwifery students' emotional health and wellbeing through the concepts of containment and reciprocity (Thelwell et al, 2017), a striking aspect of particular significance for student midwives transitioning to registration in a post-pandemic health service.
The aim of this study was to evaluate the provision of Solihull Approach training in the undergraduate programme of midwifery education. The objectives were to:
Methods
A mixed-method evaluation study using pre- and post-test questionnaires was chosen to enable capture of students' opinion and inform educational design. The study commenced in March 2020, with both training days completed prior to the onset of social restrictions because of the COVID-19 pandemic.
Sample
Final year BSc midwifery students (n=24) were the population for the study; this was a convenience sample of students from the authors' university. This cohort had insight into the structure of the curriculum, as they had reached the last 6 months of their undergraduate midwifery programme. Furthermore, they were considered to have had the most experience of the application of the Solihull Approach in clinical practice.
This range of student experience coincided with the development of a new midwifery curriculum and therefore was of important relevance for informing curriculum development and strengthening the public health role of the midwife (Meegan, 2020). Students were recruited via the student email system. Students who provided written informed consent prior to the first training day and attended both training days were subsequently included in the pilot study.
Training days
As a result of the nature of the Solihull Approach, the focus on parental and personal emotional mental health and wellbeing and the risk of distress, two experienced Solihull Approach trainers facilitated each session. Those providing the training were either a registered midwife, health visitor or midwifery lecturer registered as Solihull Approach trainers. The 2-day training course was completed in accordance with the Solihull licenced programme (Solihull Approach, 2024).
Data collection
Pre- and post-training questionnaires were adapted from a validated tool (Lander, 2008) used in previous evaluation studies in the School of Nursing and Midwifery (Hughes et al, 2014; Anderson et al, 2017). Minimal changes were made other than adjustments to the wording to reflect the nature of the topic of investigation. The pre-test questionnaire provided baseline information on students' awareness, knowledge and experience of the Solihull Approach in clinical practice and provided a comparative baseline on perceived confidence. The pre-test questionnaire comprised five questions: two used a Likert scale and three were open ended. The post-test questionnaire comprised of 11 questions: four used a Likert scale, six were open ended and one offered a choice of one of four options.
Students who consented to participate were provided with the pre-test questionnaire before the first training session, which were completed anonymously. The post-test questionnaire was sent via Survey Monkey following participation and full completion of the 2-day training. Responses were anonymous. The researchers forwarded the link for the anonymised post-test questionnaire to participating students 2 weeks following completion of the second training day. Reminder emails were sent at 7 and 14 days respectively. Responses were received by mid-April 2020.
Data analysis
Descriptive statistics were used to analyse the data from final year BSc midwifery students, with thematic content analysis of free text data used to identify emerging themes, guided by Braun and Clarke (2013).
Ethical considerations
Faculty Research Ethical Committee approval was granted (Approval number: MHLS 19_25). All eligible students were sent a participation information leaflet and consent form before data collection. Only those who provided written informed consent before the first training day were included.
Results
A total of 16 final year BSc midwifery students completed both questionnaires. In the pre-training questionnaires, all students indicated that they had some level of exposure to the Solihull Approach in clinical practice; for most students this was in community clinical practice or during their antenatal placement if they had the opportunity to work alongside the parent education midwife.
While participants had some experience of contributing to parenting preparation using the Solihull Approach with registered midwives, most indicated a lack of confidence in their knowledge and ability to support parents on their emotional journey to parenthood. Participants' expectations of Solihull Approach Antenatal Foundation Training was to learn more about the approach and gain confidence in providing it in clinical practice. Additionally, students were keen to enable a more active role in providing parenting education in community-based clinical practice. Their responses to the pre-test questionnaires can be seen in Table 1.
| Question | Response, n=16 |
|---|---|
| Do you feel confident supporting parents on their emotional journey to parenthood? (1-not at all; 7-very much) | Seven students scored 4, nine scored 5, demonstrating a reasonable level of confidence. Qualitative comments suggested students desire greater confidence |
| Do you feel confident in your current level of knowledge in relation to the factors that affect the quality of the parent–child relationship? (1-not at all; 7-very much) | Two students scored ≤3, eight scored 4, six scored 5, demonstrating a reasonable level of confidence. Qualitative comments suggested students desire greater knowledge and understanding |
| Have you had any experience of the Solihull Approach to parenting prior to today? | All students indicated that they had some level of exposure, either in their community or antenatal placement allocation |
| What are your expectations of Solihull Approach training? | Two main themes: achieve greater understanding of the parent–child relationship, learn how to support parents on their emotional journey to parenthood |
| What do you hope to gain from Solihull Approach training? | Unanimous responses indicated a desire for increased knowledge and understanding of theoretical underpinnings of the training and achieving greater confidence in delivering it while supporting parents in clinical practice |
In the post-training questionnaire, themes included the perceived benefits for clinical practice; increased level of knowledge and confidence; increased recognition of the public health role of the midwife; and how best to integrate the timing of the training in the undergraduate curriculum.
Benefits for clinical practice
Most free-text responses related to the benefits for clinical practice regarding how participants' increased level of knowledge and confidence would ultimately benefit care provision for mothers and their families. Participants also noted how, as students about to make the transition to newly qualified midwife, improved knowledge and confidence would also impact their role as public health practitioners and personal containment.
‘Even more awareness of the importance of antenatal education … ideas on how to teach/engage/support parents’.
‘How to teach antenatal care and the meaning of containment’.
‘Learning how important it is to engage and respond to a baby right from utero to help it develop and then how to support parents’.
‘Gained skills in how to articulate this information to new parents’.
‘Increased level of confidence in preparing for the transition to newly qualified midwife’.
Increased knowledge and confidence
In relation to achievement of knowledge, 90% of participants scored ≥5, with 70% scoring ≥6. The free-text comments demonstrated the range of learning achieved. This increased knowledge translated to perceived confidence in providing Solihull Approach training in clinical practice.
‘Increased self-awareness; knowledge of emotions and behavioural skills in articulating emotional aspects of parent education’.
‘Gained knowledge from theory/concept of the approach’.
‘Greater confidence in discussing baby brain development with women’.
Increased recognition of the public health role of the midwife
When asked how relevant the training and the Solihull Approach was to midwifery practice, 60% of participants responded with ‘very much’ (7). Additional comments in this section focused on the opportunity to view parent education from a public health perspective and appreciate the midwife's role, recognising the value of antenatal education and how it related to early intervention.
‘Use Solihull Approach in all areas of midwifery practice when talking with women’.
‘The knowledge that I need to reach others as a midwife in early intervention’.
Timing in the curriculum
The participants unanimously indicated that they felt that training in the Solihull Approach should be integrated in the pre-registration midwifery education programme. However, results were ambiguous when asked which year of the programme it should sit with; 50% felt that it should be provided from the outset in the first year of the educational programme.
Discussion
The public health role has long been recognised as an integral component of the role of the midwife (Crabbe and Hemmingway, 2014; Gomez, 2016; Royal College of Midwives, 2017; Cutter, 2021), a role that has been strengthened in the standards of proficiency for midwives (NMC, 2019) and emphasised by the Royal College of Midwives (2017). Respective government maternity strategies have also emphasised the importance of the midwife's role as a public health practitioner (Department of Health, 2012; 2016; National Maternity Review, 2016; Scottish Government, 2017; Welsh Government, 2019).
The contribution that midwives make to the welfare of families is highly valued and the public health role of the midwife has been increasingly enhanced in midwifery practice (McNeill et al, 2012; Gomez, 2016). In particular, the importance of early intervention to improve public health outcomes has been recognised with the implementation of universal care during the antenatal period and recognition of the importance of emotional health and wellbeing in the transition to parenthood. A significant body of evidence supporting early intervention is now available through the Early Intervention Foundation (2021). Further recent evidence from the Academy of Medical Sciences (2024) emphasises the importance of laying the foundation for adult health through early years intervention.
Advancing knowledge of the impact of epigenomics on future health further emphasises the importance of the midwife's role in public health and the need to be alert to the potential impact of epigenetics on health, for example, in relation to attachment (NMC, 2019; Darling Rasmussen and Storebø, 2021). Supporting learning about the theory and practice of public health interventions is crucially important in undergraduate midwifery education programmes to ensure that registered midwives are ready to fulfill the full scope of public health practice from the point of registration. This pilot evaluation study of an innovative initiative contributes to an understanding of how this might be manifested in midwifery education programmes, particularly in relation to the benefits for practice, and the impact of education related to knowledge, confidence and increased recognition of the public health role of the midwife.
Contemporary midwifery practice entails caring for women with increasingly complex pregnancies and births (Renfrew et al, 2014; NMC, 2019). Solihull Approach Antenatal Foundation Training offers midwives an additional tool and skillset to support the emotional health and wellbeing of women and their families across the childbirth continuum, irrespective of the level of complexity, promoting the transition to parenthood (Thompson and Summers, 2018). Maternal mental health has been recognised as a contributing factor to the development of attachment in the mother–infant dyad. Infants of mothers with reduced emotional availability may lack the reciprocal connection that enhances the development of attachment and the sequelae of events that follow may have a negative impact on the infant's emotional and psychological development, which can have long-lasting impact on their wellbeing in later life (Sutton, 2016; McLeish and Redshaw, 2017; MacMillan et al, 2020; Galbally et al, 2023). Therefore, building positive relationships between mother/infant/family is key to population health and a preventative mechanism for promoting health (Rheeston, 2018).
The impact of the pandemic has demonstrated the importance of resilience for both qualified and pre-registration midwives. Solihull Approach Antenatal Foundation Training not only provides preparation for mothers transitioning to parenthood but also tools, such as resilience, for student midwives transitioning to the role of newly qualified midwives. The notion of resilience in midwifery practice has been gaining momentum and is considered a necessary attribute for professional practice (Crothers et al, 2016; Clohesy et al, 2019; Baldwin et al, 2022; Williams et al, 2022).
In Northern Ireland, the concept of early intervention as an approach to improving health outcomes for children, and the central role of families in providing physical and emotional support, thus ensuring health and wellbeing, has been well accepted. Strategic plans have been developed and implemented over the last decade such as Families Matter (Department of Health, 2009) and Healthy Child, Healthy Future (Department of Health, 2010). The latter plan implemented the framework for the Universal Child Health Promotion Programme in Northern Ireland from pregnancy through to 19 years and outlined the assessments and interventions relevant to all families, including those with additional needs, children in need and children with complex and/or acute needs (Department of Health, 2010).
An important component in facilitating Solihull Approach training is sustainability. To that end, all available midwifery lecturers completed Solihull Approach Antenatal Foundation Training in 2018. Three midwifery lecturers have since completed the Solihull ‘train the trainer’ programme and can facilitate training for student midwives in partnership with clinical midwives who facilitate training in clinical practice. New midwifery lecturers who have not completed Solihull Approach Antenatal Foundation Training will be able to avail of training alongside MSc Midwifery cohorts.
The Solihull Approach is a licensed programme and therefore there is a limit to the amount of creativity or diversity that can be used for delivery of the programme. For example, the recommended group size of 12–15 participants per 2-day programme has an impact on logistical planning and incorporation in an already intense programme of education for a cohort of 60–80 students. However, the perceived benefits of integration in the undergraduate programme outweighed the resource intensity required to successfully run the programme.
Designing a new curriculum offered the opportunity to review integration of Solihull Approach Antenatal Foundation Training in the public health theme across the 3-year BSc programme. The Solihull Approach training content was mapped to the learning objectives and content for each of the public health modules (one in each year of the BSc programme). Following discussion with the Solihull Team, an agreement was reached whereby the content would be delivered across the 3-year programme in the respective public health modules without detriment to the fidelity of Solihull Approach Antenatal Foundation Training, thus easing the burden of resource intensity. The smaller size cohort for the MSc Midwifery programme of education allows for the delivery of Solihull Approach Antenatal Foundation Training in its original format of a 2-day programme.
Implications for practice
Further to the outcomes of the study, Solihull Approach training has been integrated in the pre-registration undergraduate midwifery education programme and introduced earlier in the programme. There is the potential to incrementally build on this foundational knowledge and understanding and include further tiers of learning, such as the ‘getting ready for baby’ learning package or signposting students to further Solihull online learning resources to advance their knowledge. Solihull Approach training will continue to be evaluated in the undergraduate midwifery education programme. The impact of including the training in pre-registration provision and the students' application of Solihull Approach training in clinical practice warrants further investigation.
Limitations
The small sample size reduced generalisability and further evaluations will be undertaken as Solihull Approach Antenatal Foundation Training is rolled out across the curricula. The impact of COVID-19 on undergraduate education and the move to online delivery was not conducive to providing the training because of the emotive nature of content and ability to appropriately support students who may become distressed. Therefore, the full integration of Solihull Approach Antenatal Foundation Training in the undergraduate curriculum was delayed until face-to-face delivery resumed.
Conclusions
The findings of this pilot study appear to support the integration of Solihull Approach Antenatal Foundation Training in undergraduate midwifery education. The four themes emerging from the data demonstrate that the training is relevant for students' experience of midwifery practice and helps midwifery students feel better prepared for the transition to newly qualified midwives. Having completed this innovative training programme, students will enter the midwifery practice team at the point of registration with increased knowledge and parenting education skills, in addition to an enhanced level of confidence when delivering parenting education classes.
Facilitation of the pilot evaluation has not been without challenges in the pre-registration midwifery curriculum. The logistics of running a uniquely licensed training package alongside an already packed curriculum agenda created concern regarding the available resources and additional burden for students. However, with the introduction of the new standards for midwifery education, designing a new pre-registration curriculum offered a unique opportunity to integrate Solihull Approach Antenatal Foundation Training and map the training sessions to the public health learning outcomes, thereby addressing the challenges efficiently. Public health has been strongly emphasised as an important component of the new curriculum and, as such, Solihull Approach Antenatal Foundation Training now sits neatly in the student midwife's learning journey. Ongoing evaluation of Solihull Approach Antenatal Foundation Training as it is rolled out across the new curriculum will testify to the effectiveness of this unique and innovative learning opportunity.


