Fetal heart rate monitoring in labour aims to identify fetuses who may be developing hypoxia, and allow timely intervention to prevent long-term poor neurological outcomes (Alfirevic et al, 2017). For most women who are healthy, have had normal pregnancies and no risk factors, evidence-based recommendations from the National Institute for Health and Care Excellence (NICE) are that the fetal heart rate can be monitored through intermittent auscultation every 15 minutes, using a Pinard or hand-held Doppler device (NICE, 2014). Continuous electronic fetal monitoring involves the use of two transducers (one to monitor the fetal heart and one to monitor uterine activity) attached to the woman's abdomen via leads and connected to a cardiotocograph machine (CTG). A continuous record of the fetal heart and uterine activity is recorded and printed. Continuous electronic fetal monitoring is recommended for women who enter labour with an underlying medical or fetal condition or in the event that complications develop during an otherwise low-risk labour. In the UK, approximately 60% of women will have continuous electronic fetal monitoring at some stage of their labour (NICE, 2014).
The advantage of electronic fetal monitoring is that the fetal heart and uterine activity can be continuously recorded, showing trends over time. The CTG can then be systematically assessed and categorised per a set of criteria (NICE, 2014) and further assessment undertaken (such as fetal blood sampling or expediting the birth). Disadvantages are that clinical staff may focus on the recording and interpretation of the CTG rather than the woman, and that there are likely to be more interventions (Alfirevic et al, 2017). In addition, the leads prevent the woman from moving freely, changing position, or using the bath or pool. While women may derive a sense of reassurance from increased surveillance and hearing the fetal heart continuously, they also view it as being associated with technical medicalisation of birth and enforcing immobility and discomfort (Mangesi et al, 2009; Barber et al, 2013).
Telemetry
Electronic fetal monitoring by telemetry also employs two transducers on the abdomen, but information about the fetal heart and contractions is transmitted wirelessly. The woman is freely mobile and as the transducers are waterproof, can be immersed in water. Telemetry machines can be purchased in addition to conventional electronic fetal monitoring equipment, at an added cost, as well as being available as an integrated part of fetal heart rate monitoring equipment.
A meta-analysis of 6 randomised controlled trials ranging from 1978–2004 found no difference in the mode of birth or length of labour for women monitored using telemetry, compared with women monitored using conventional CTG (NICE, 2014), although use of telemetry was associated with lower rate of epidural use compared to conventional CTG (NICE, 2014). The majority of the literature used in this meta-analysis is outdated: much of the telemetry described required a fetal scalp electrode to be attached and for women to carry extra equipment around. The UK intrapartum guidelines (NICE, 2014) formally recommend that all women having continuous fetal heart monitoring in labour should be offered telemetry but caution that, given there is no recent peer-reviewed literature evaluating the use of telemetry, further research should be undertaken. Future research should explore any effect on neonatal outcomes, duration of labour, and use of pain relief, as well as evaluating women's and midwives' experiences of telemetry during labour (NICE, 2014). A recent service evaluation has been performed in one UK maternity unit following the introduction of 10 telemetry units to support active birth for all women (Morrall and Beach, 2017). Following the introduction of wireless monitoring, the normal birth rate increased over a 3 year period from 59.9% to 64.7%, and both staff and women evaluated the project positively.
Despite the recommendation from NICE, there was no indication of the number of maternity units in the UK that have telemetry, how often it is used and in what circumstances. This survey therefore aimed to gather information from maternity units on whether they offered telemetry in line with guidelines, and to gain a sense of how telemetry was used, the women for whom it was used and whether there were any perceived advantages or disadvantages to using telemetry for women in labour. A national online survey was therefore developed and sent to all maternity units in the UK.
Methods
An online survey method was chosen for practicality, as it was thought that responses would be reasonably rapid once emails had been received. Ethical approval was not required. Given that there was very little contemporary literature on the use of telemetry to inform question development, the survey questions were developed pragmatically by the authors, drawing from clinical experience and expert opinion. Questions were entered into the online survey platform (surveymonkey.com). There were 20 questions in total; the initial 5 were closed geographical and demographic questions such as size and location of the maternity unit and the role of the health professional completing the questionnaire. The following 15 questions related directly to the use of telemetry; 8 of these questions also had space for free text comments and the final question was for any further comments the respondent wished to make.
Sample and data collection
The survey was undertaken over a 12-week period from November 2013–February 2014. Email addresses for Heads of Midwifery from 168 maternity units in the UK were obtained from local supervising authority midwifery officers, and a covering letter detailing the study, including contact details and a link to access the survey, was sent. In January 2014, a further email was sent to units that had not responded. Heads of Midwifery were asked to forward the survey on to another member of staff if they were unable to complete it themselves. A further email was sent to all consultant midwives in the UK with the link to the online survey, in order to increase uptake. Data were collected and managed via the online survey tool and response rates checked regularly.
Data analysis
Once the survey had closed, data were checked to ensure that units had not responded twice. Data were analysed descriptively and presented in tables. Free text content was thematically analysed using simple tables to allow collation of topics and development of themes.
Results
The response rate for the survey was 62% (n=104). Respondents were Heads of Midwifery (29%), consultant midwives (20%), midwifery matrons (19%) and senior midwives (32%). There was a spread of responses from throughout the UK including Wales, Northern Ireland and Scotland, with the highest number of responses coming from northwest England (13%), southwest England (14%) and London (14%). Of the units responding, 46% cared for >5000 women per year, 32% between 3000 and 5000 per year, 21% between 1000 and 3000 per year and 1% for fewer than 1000 women per year.
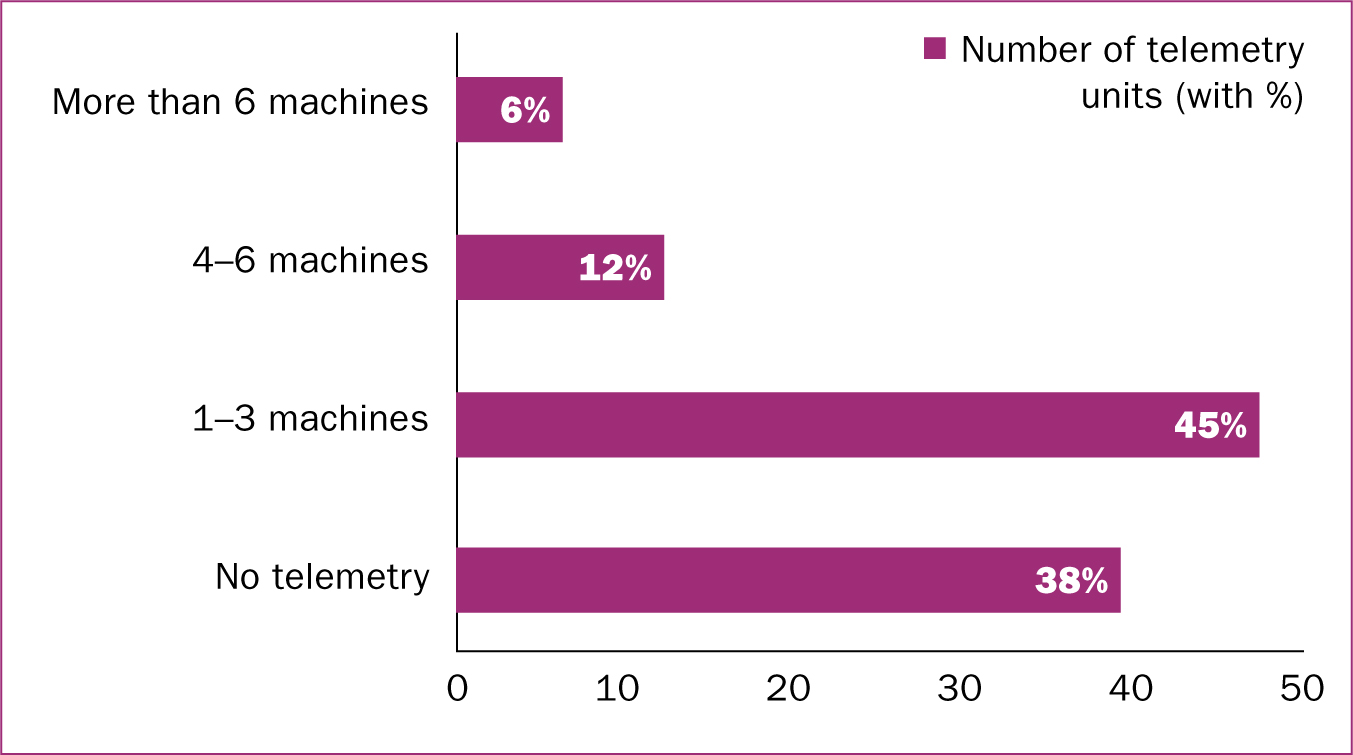
Telemetry provision, frequency and guidelines
Responses for how many telemetry machines units had for providing continuous electronic monitoring of the fetal heart in labour are presented in Figure 1. In total, 38% (n=39) of maternity units did not have the facility to monitor with telemetry, 45% (n=47) had between 1 and 3 machines, 12% (n=12) had between 4 and 6 machines, and 6% (n=6) had more than 6 machines. Overall, 63% (n=65) of responding units could provide telemetry for women in labour. One maternity unit responded in free text about the number of telemetry machines available:
‘We have 18 units for intrapartum, all have telemetry, we have no others available for intrapartum.’ (Obstetric and alongside maternity unit, >5000 births per year)
Although there were 65 maternity units with telemetry, not all of the units responded to all of the questions (ranging from 59–62). The majority of responding maternity units that could provide telemetry (n=46/62; 74%) had been using it for more than 1 year. Of the 39 maternity units that did not have telemetry, 50% (n=18) were intending on purchasing in the next 6 months. Some maternity units had trialled machines that they were going to purchase, while others were raising business cases for purchase.
In order to get a sense of how often telemetry was used, maternity units were asked how many women per week would use telemetry in labour and 62 out of 65 units with telemetry responded to this question. 5% (n=3) stated that no women used telemetry, 50% (n=31) stated that between 1 and 4 women would use it per week, 21% (n=13) stated between 5 and 10 women per week and 24% (n=15) stated more than 10 women per week. Of responding maternity units with telemetry, 52% (n=32) had guidelines specifically related to telemetry and monitoring the fetal heart, with three free text comments stating that their guidelines were only related to electronic fetal monitoring and not telemetry specifically. A large proportion (82%; n=50/61) of maternity units with telemetry machines stated that the machines could move around the unit rather than being allocated to specific rooms. Some machines remained permanently in rooms with pools and 97% (n=59/61) of units with telemetry had a pool available for use. Maternity units with telemetry were asked what proportion of women using telemetry would also use the pool; 75% (n=44/59) of units stated that less that 25% of women would use the pool with telemetry.
Issues with telemetry machines
Maternity units were asked whether they had experienced any problems with telemetry monitoring and 52% (n=32/61) of units stated that they had. There were 28 free text comments, including those related to transducers breaking or being lost and expensive to replace, loss of contact resulting in poor quality recordings, and issues with coverage and connectivity. The most frequently cited problem was that there were occasions where transducers were not being returned for charging and so not ready for use.
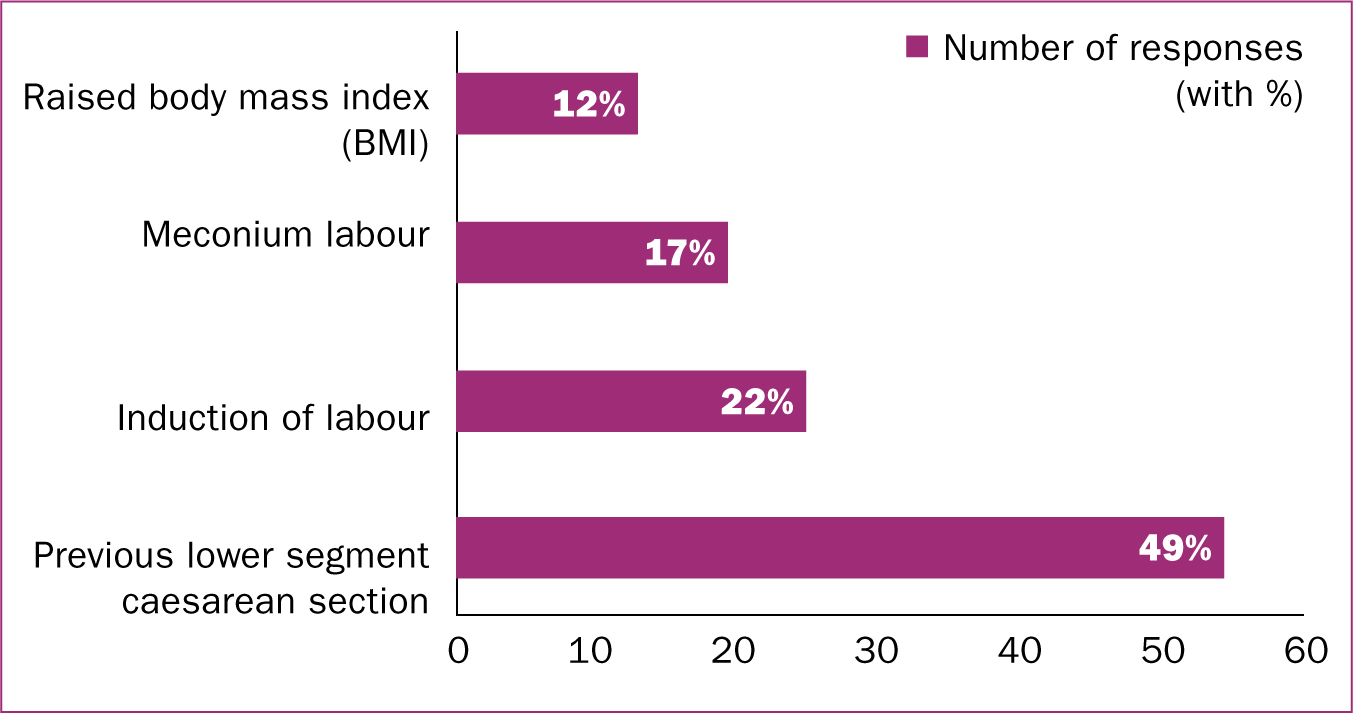
For whom is telemetry used?
Responses to the question ‘For which women is telemetry most used?’ are given in Figure 2. Respondents could give more than one answer and, in total, 112 responses were provided. Women who had had a previous caesarean section were the group for whom telemetry was used the most (n=55; 49%). There were 17 additional free text responses, which commonly said that telemetry was used for any women requiring continuous fetal heart rate monitoring who wished to be mobile or wished to use the pool. As one free text comment explanined:
‘We use telemetry as standard for women requiring electronic fetal monitoring.’ (Obstetric, alongside and freestanding maternity unit, >5000 births per year)
Of the responses received, 12% (n=13) identified women with a raised body mass index (BMI) as a group for whom telemetry was used.
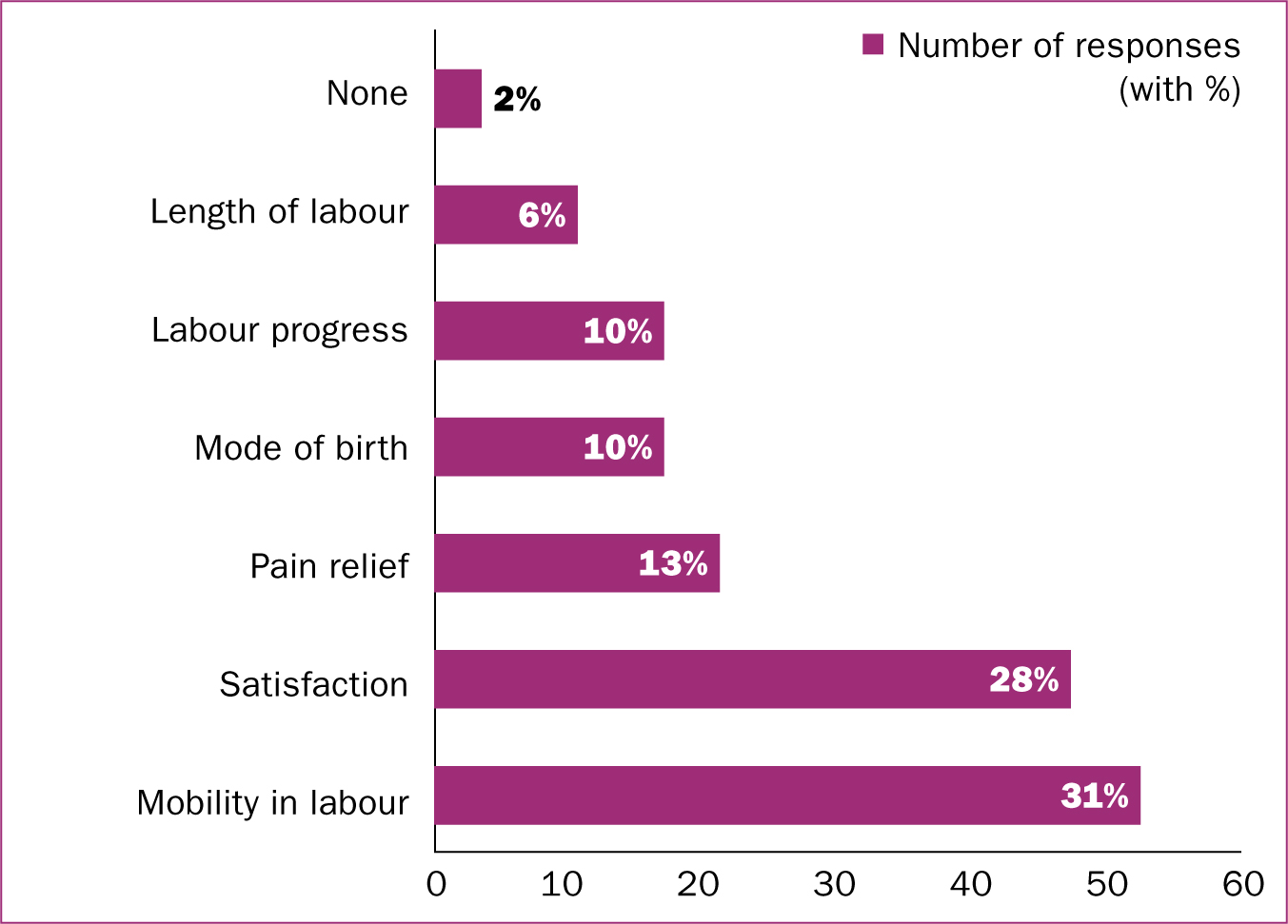
Influence on birth
Responses to the question ‘In your experience, which labour outcomes are positively influenced using telemetry?’ are given in Figure 3. The phrasing of this question may have produced subjective responses but the authors felt that, as senior midwives were completing the survey, their knowledge and experience about perceived influences on outcome would be beneficial to gauge. More than one answer could be given, and a total of 166 responses were given from 59 maternity units. Mobility in labour (n=52; 31%) and satisfaction with labour experience (n=47; 28%) were given as the top two outcomes that respondents felt telemetry could influence. Comparatively smaller numbers were given for length of labour (n=10; 6%), use of pharmacological pain relief (n=21; 13%), mode of birth (n=17; 10%) and labour progress (n=16; 10%). Maternity units that had telemetry were asked if they collected any data on its use and only 10% (n=6/61) of units did. These units had not been collecting data for long and did not have any findings that were able to be shared with the authors.
General comments
Finally, maternity units were asked if they had any additional comments to make about the use of telemetry for continuously monitoring the fetal heart in labour. A total of 23 comments were received. Some of the comments related to telemetry being available but not being embraced by staff or embedded well within the unit. One respondent commented that:
‘We have had problems with the telemetry, and the midwives don't like it, though not sure why’ (Obstetric unit, >5000 births)
One comment highlighted that staff were not confident with using telemetry. Comments also related to capabilities of the machines including difference between models, fetal scalp electrode facility, and the difficulties of monitoring women with a higher BMI.
Most free text comments were positive, and included themes of getting funding to introduce more, encouraging staff to use telemetry, promoting its use as standard and responding to women's choice. One respondent stated:
‘Telemetry has enabled us to provide the same birth choices for women with risk factors as those who are low risk. High risk women in the past have been disadvantaged—but thankfully that is now not the case. We are changing any monitor that needs replacing to telemetry to improve choices for women.’ (Obstetric, alongside and freestanding maternity unit, 3000-5000 births per year)
A further response confirmed intentions to purchase more telemetry in the future:
‘We plan to introduce more units in the next year as this is what high risk women want to give them control over their delivery experience.’ (Obstetric and alongside maternity unit, 3000–5000 births per year)
Discussion
Limitations of this survey are that the response rate meant that only 104 maternity units provided responses, however, a 62% response rate is comparable with a recent national maternity surveys (Richens et al, 2015; Mills et al, 2016) and more favourable than others (Cooke et al, 2011; Jokhan et al, 2015). This online survey was designed as a snapshot look at the availability of telemetry within UK maternity units, to give a sense of how and when it was used, and any perceived advantages or disadvantages. It was not designed to investigate barriers or facilitators to the use of telemetry, including organisational and cultural factors and training for midwives, in detail, and future in-depth research is needed in this area. The survey was also not able to capture views and preferences of women on the use of telemetry and this is an additional area for further investigation.
The main strength of this study is that it is the only survey done of contemporary telemetry use in UK maternity units. It provides an insight into how telemetry is used and highlights a potential ‘turn-of-tide’ in the way that women are, and have the potential to be, continuously monitored in labour. There was excellent geographical spread of respondents, giving confidence that the survey could determine a realistic picture of telemetry use in maternity units in the UK. The survey responses from more than 100 maternity units indicate that telemetry is available in a majority and that many other maternity units are looking to purchase more to provide increased choice for women with more complex pregnancies and labours. It was evident from the survey that telemetry was used for the most common reasons for a woman to be continuously monitored, such as meconium, previous caesarean section, and induction of labour. Telemetry is also being used to monitor women with a raised BMI. While there is no clear guidance on obesity and continuous fetal heart rate monitoring (Centre for Maternal and Child Enquiries and Royal College of Obstetricians and Gynaecologists, 2010), it is evident that telemetry is being used for these women and aligns with telemetry use in the literature on how to increase normal birth rates for obese women (Swann and Davies, 2012; Kerrigan et al, 2015).
Some of the problems with telemetry were also highlighted, and there was an indication that issues such as transducers not being left to charge, or problems with the signal, may be affecting how units with telemetry are able to embed it. One of the assumptions about telemetry is that women will be more upright and mobile in labour, which was mirrored in the free text responses that concerned the benefits of telemetry. Both mobility and use of a birthing pool in labour have been shown to reduce length of labour and use of pharmacological analgesia (Cluett et al, 2009; Lawrence et al, 2013); however, there is no evidence that telemetry means that women are more mobile and upright during labour, or use a birth pool more often, and more research is warranted in this area. Satisfaction with labour experiences also featured highly; an indication that the ability to be more mobile leads to increased satisfaction.
Conclusion
This survey showed that 59% of responding maternity units had telemetry to monitor the fetal heart in active labour, and 49% of units without telemetry were planning on purchasing some in the near future. The benefits that maternity units saw for women by providing telemetry were clear, primarily regarding providing choice for ‘high-risk’ women, and it is recommended that maternity units continue to provide this option. Further research is planned by the authors to broaden the understanding of telemetry use and to investigate whether telemetry has an effect on control or satisfaction in labour, mobility, and labour outcomes such as length of birth and use of regional anaesthesia.

