The diversity of the midwifery education workforce is of continuing concern (Royal College of Midwives (RCM), 2023a), particularly in the light of ongoing MBRRACE-UK (2022; 2023a, b) data relating to outcomes for women, and their families and babies. The evidence shows that representation at every level is key to improving outcomes. This article considers the influence of institutional racism on the practice of global majority academics and students, and how we, as midwifery educators, have (or have not) begun to embrace decolonisation of the midwifery curriculum. The demographics in the existing workforce and the benefits of racial diversity for students, staff and NHS service users are discussed, as well as how leaders in higher education can respond to racism to create allyship and the necessary culture shift to empower global majority academics.
The term ‘global majority’ is used in this article to collectively refer to people from Black, Asian, brown, dual heritage and other groups, although when quoting statistics, the terminology of the various reports is used. The term global majority disrupts narratives that suggest people from marginalised groups are less than, especially the term Black, Asian and minority ethnic (Campbell-Stephens, 2020). It also encourages people from this background to see themselves as belonging to the global majority, where identity transcends geography and does not exist solely in relation to dominant whiteness. The authors of this article are aware that they are both White and have advantages afforded to them because of this. The authors do not pretend to fully understand or represent the views of the global majority. They are grateful for the time spent by global majority colleagues in helping the authors better understand some of the issues discussed below. The authors champion diversity in their staff and student body and are educating themselves and others in anti-racist practices; for example, we have joined or attended our university's anti-racist collective, read books and challenged peers on their terminology use assumptions.
A profound lack of diversity in the midwifery profession
The RCM has been sending freedom of information requests to UK universities since 2010. However, their request in 2023 (which formed the basis of the subsequent report on which this series is based) was the first time that the ethnicity of midwifery educators was included (RCM, 2023a). There has been considerable evidence of inequalities in maternity outcomes for women from global majority backgrounds since Knight et al (2009) and the events of 2020 (the COVID-19 pandemic and murder of George Floyd), which highlighted structural and institutional discrimination (MBBRACE, 2022; 2023a, b). Given that, it is surprising that this information has not been requested previously.
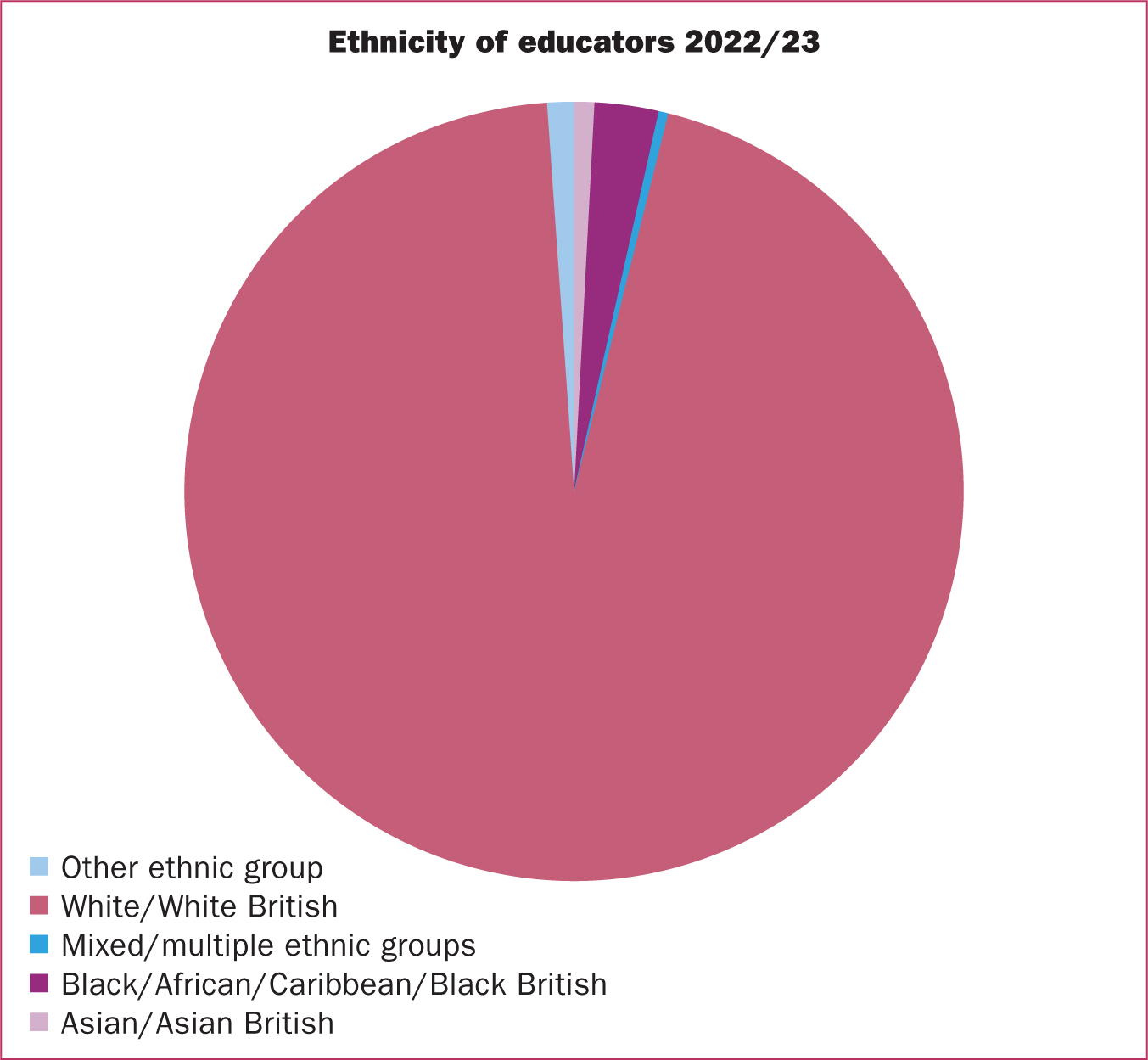
Despite the greater national awareness and action to address inequalities, some universities withheld their data for this diversity question. The universities used Section 40 (2) of the Freedom of Information Act, which states personal data can be withheld if it contravenes data protection principles. The number of universities who withheld the data is not stated. Of those that replied, 95% of midwifery educators were White (RCM, 2023a). A pie chart (Figure 1) was used to represent the ethnicity of the midwifery educators in the report, but no other statistics are offered (RCM, 2023a). From the size of the pie chart slices, the 5% of midwifery educators from global majority backgrounds predominantly identify as Black/African/Caribbean/Black British, followed by mixed/multiple backgrounds, with Asian/Asian British represented least.
The NHS (2023) has a more diverse staff body for all professionally qualified groups (doctors, paramedics, healthcare scientists, nurses and midwives), with 31.3% from Black, Asian and other demographics. There are slightly more global majority nurses (32.6%) and significantly greater representation among doctors (49.9%). By comparison, the NHS (2023) global majority midwifery workforce is 13.3%, nearly three times that of midwifery academics. Black midwives make up 7.8%, followed by midwives from an Asian background (2.5%), mixed heritage (2.1%), Chinese (0.2%) and other ethnicities (0.6%).
It is not just the midwifery profession that has fewer global majority academics in higher education than clinical practice. The Council of Deans for Health (CODH, 2020) noted that the diversity of academics in all healthcare professions was lower than in clinical practice. Their survey was returned by 61% of universities, but only 58% (49 of the 84 universities who are members of the CODH) replied to the individual staff demographic data. There were noteworthy differences between the professions and four countries of the UK; however, a caveat is given that because of the response rate, this does not provide a complete picture. Those from global majority backgrounds comprised only 7.9% of their sample of 6830 healthcare professional academics, with the largest group from Asian/British Asian backgrounds (3.5%), then Black university academics (2.3%). The CODH report compared the higher education staff demographics more broadly and found that 22.6% of higher education academics were from global majority backgrounds, compared to the 7.9% in academic healthcare professions.
Recruiting midwifery staff to higher education was not reported as being as difficult as recruiting to nursing or allied healthcare professions (CODH, 2020), despite the need to attract academics from under-represented groups into academia. This is especially important for midwifery when the proportion of global majority academic midwives is lower than for other healthcare professions and higher education generally. Midwifery needs to move from being a predominantly White profession to having greater diversity at all levels: students, clinical staff, managers and in higher education. The lack of representation of global majority midwifery academics may be a limiting factor in recruiting this demographic of student and the students' experience in clinical practice and university may be negatively influencing the likelihood of these midwives progressing into academia, as the evidence demonstrates (Pendleton et al, 2022; Okiki et al 2023a, b; Gnanapragasam 2024a, b).
Individual, institutional and systemic racism
Education is said to be transformational, for the individual accessing it and for its benefits for society (Williams and Cochrane, 2010). This Sapientia section of the British Journal of Midwifery aims to bring wisdom and good sense to the profession (McEwan and Editorial Board, 2023). To change the experience and outcomes of people from a global majority background, whether they are accessing education intending to become a midwife, teaching the future workforce or a woman experiencing pregnancy and birth, there is a need for a shared understanding of racism in all its forms, so that anti-racist practice becomes the collective norm. Anti-racist practice is both an individual and organisational process of identifying and eradicating racism by identifying the root causes in systems and organisational structures, policies and practices so that power is shared equitably (Miller, 2021).
If an individual holds the belief that one group of people are inherently superior to another group, particularly an ethnic group, this is classed as individual racism. Most people understand this form of racism, especially if it is overt. Three other terms, institutional, structural and/or systematic, are often used interchangeably. Institutional racism manifests as different outcomes for certain groups in society. While there are nuances between them (Braveman et al, 2022), it does not particularly advance the discussion here.
Institutions, such as universities, have been examining and addressing policies and practices to reduce inequalities between groups, such as recruitment practices and what is taught in the midwifery curriculum (RCM, 2023b). However, sometimes the effects on certain groups are so stark and profound that groups are systematically or structurally disadvantaged. Systemic racism emphasises these systems: legal, education, healthcare and criminal, often all systems are involved. Systemic racism also includes the structures that operate at an institutional level (laws, policies and entrenched norms) that enable racism to exist (Braveman et al, 2022). The development of systemic racism is often cumulative, involving history, culture, beliefs and interactions with institutions. Systemic racism has been identified as the root cause of the difference in pregnancy and birth outcomes for women from global majority backgrounds in the UK (MBRACE-UK 2022; 2023; Birthrights, 2022).
Systemic racism may also explain why there are so few global majority midwifery academics. To become a midwifery academic, prospective students need first to choose midwifery (whether this is the direct entry route or shortened course for registered nurses), enrol as a student, graduate and choose an academic career path. This article explores the contemporary evidence from potential applicants to midwifery, midwifery students and newly qualified staff before attending to the research on academics to examine barriers to progression.
Global majority midwifery students' experiences and outcomes
Barriers exist at the very beginning of entry to a midwifery career pathway. Okiki et al (2023a) conducted a survey of 101 global majority midwifery candidates and 314 white candidates on direct entry programmes at three universities in the southeast of England. Their quantitative survey data were triangulated by focus group interviews with 13 global majority midwifery students and one newly qualified midwife. The authors found some significant differences between the two groups of applicants, including the choice, career path and determination needed to pursue midwifery. Global majority applicants were less likely to know about midwifery as a career than their White counterparts, and there was some global majority community stigma regarding choosing midwifery as a profession, although the participants could not articulate the cause. Additionally, global majority families were less likely to be encouraging of midwifery as a career choice.
During the application process itself, there were barriers for global majority applicants (Okiki et al, 2023a). There were no or not enough global majority academics at the university to cover open days and interviews, meaning that global majority applicants did not see midiwfery staff represented. This was a barrier to applicants feeling they belonged at the university. There was a lack of diversity in the existing student body and the interview process was not seen as equitable for all applicants. The discussion noted institutional racism as a barrier to recruiting global majority midwifery students (Okiki et al, 2023a). However, the authors of this article would argue that this is structural racism, as the effects are cumulative and cultural, as well as institutional.
Once recruited to the course, global majority midwifery students had to navigate institutional whiteness (Okiki et al, 2023b). The 13 midwifery students and one preceptor were asked how their ethnicity affected their experiences in university and in placement. The strength of the findings, of being an outsider, discrimination and racism, are palpable in the direct quotes and analysis. The participants also witnessed racism directed at women and families in clinical practice. Participants were wary of reporting this for two main reasons; not knowing where to report it and feeling fearful of repercussions. Midwifery academics too were reportedly unhelpful, dismissive or lacked the capacity and structural mechanisms to respond. There were some positive findings, with the importance of allyship from White and other global majority midwives and students advocating for change and challenging the status quo. Favouritism from lecturers and practice supervisors towards White students was noted. There is a clear need for midwifery academics and placement facilitators to openly discuss racial inequalities and address discrimination (Okiki et al, 2023b).
Gnanapragasam (2024a) explored the assessment results of midwifery students in one English university. While this also derived from the south of England, it was a different region to the Okiki et al (2023a, b) studies. Gnanapragasam (2024a) found a statistically significant difference between Black, White and other ethnicities of student degree classifications. Comparing the results from 247 midwifery students, 70% of White students were awarded a First-class award compared to 34% of Black students and 52% of students from other ethnicities. The study found that something was happening during the student journey that resulted in the degree awarding gap. On reading Gnanapragasam's (2024a) paper, the authors of this article attributed this gap to grading of midwifery practice (Chenery-Morris, 2020), because the sample was from 2014–2018 when it was mandatory for all UK midwifery curricula to grade clinical practice (Nursing and Midwifery Council (NMC), 2009). While no mention of clinical grading was discussed, Gnanapragasam (2024b) covered this in their second article. Here, the analysis of practice assessments demonstrated that Black, Asian and minority ethnic students were less likely to receive a First in practice in the first year of their studies (27.8%) compared to their White counterparts (53.1%). The lower overall degree classification and likely impact of lower practice grades on self-esteem, placement experience and sense of belonging for these learners may reduce the likelihood of these midwives progressing into academic careers.
One further study examined the experiences of five Black, Asian and minority ethnic midwifery students at another English university, with similar findings (Pendleton et al, 2022). Again, there was a lack of global majority representation in their cohort, in practice and the teaching team, compounded by racist attitudes and stereotyping. This was exacerbated by the White-centric teaching materials. Collectively, these studies demonstrate that there is an issue with inclusion throughout midwifery education.
For internationally trained nurses who want to become midwives, many of whom are from the global majority (NMC, 2023), some are not eligible for the shortened midwifery course because of their visa requirements. Additionally, some internationally trained, dual-qualified nurses and midwives have only registered their nursing status with the NMC, reducing the potential pool of midwifery academics further. Anecdotal evidence from colleagues suggests the process for NMC nurse registration is better known and considered less risky than midwifery registration. Research to determine the reasons for this would aid understanding of the challenges and necessary action.
Experiences of global majority academics
The authors intended to include the experiences of global majority midwifery academics in this article, but could not identify research from this specific group. In part, this could be because there are so few global majority academics in UK higher education. However, it is also likely to be attributed to racism in action, with systemic under-representation in research of these staff experiences. However, there were many papers on Black female academics' experiences in higher education more broadly (Wright, 2007; Sang, 2018; Stockfelt, 2018). While the authors acknowledged that midwives are not exclusively female in the last article in this series (Chenery-Morris and Divers, 2024), the vast majority are. Therefore, the experiences of female global majority academics have been used as a proxy to represent some of the difficulties that midwifery academics from these backgrounds may encounter.
Being female and from a global majority increases the likelihood of discrimination from sexism and racism (Sang, 2018). The term used to describe the compounding disadvantages of multiple identities, such as disability, sexuality or socioeconomic status, is called intersectionality. The effects of these personal characteristics and experiences, intersecting with systems and structures, have been studied in nursing research, practice and education (Siira et al, 2023). Intersectionality, as a theory, lens, method or tool for research aids awareness and analysis of inequalities so that action can be implemented to address these in a more meaningful way (Siira et al, 2023).
The experiences of global majority academics resonate with those of midwifery students, despite the obvious difference between being a member of staff and being a student. Academics also experienced discrimination (Stockfelt, 2018), marginalisation (Sang, 2018), hyper-scrutiny (Wright et al, 2007) and outsider status (Bhopal, 2015). Similarly, articles summarising issues in nursing higher education described the experience of faculty from diverse backgrounds and explored strategies for improving culture and diversity (Alsulami and Sherwood, 2020). Findings demonstrated that greater faculty diversity was beneficial for all; academics, administrators and students.
Making a positive change: actions for change, allyship and anti-racist practice
Academic midwives working in higher education can improve the experiences of global majority midwifery students and outcomes for women (and influence representation in academia). This can be done by teaching a curriculum that acknowledges and explores individual, institutional, and systemic racism (Jieman et al, 2022), and that gives all students the tools to undertake inclusive, clinically relevant assessments and treatments. As a minimum, this should include recognising changes in the condition and deterioration of women and babies with darker skins (RCM, 2023b). Academics also need to listen to and follow up on all reports of racism (Birthrights, 2022; Playfair et al, 2023).
The RCM (2023b) has published an education toolkit that aims to remove the colonial lens through which most education has historically been taught in the UK. For instance, the content of key midwifery textbooks has been, rightly, criticised for presenting a light-skinned, Eurocentric White woman as the norm (Harkness and Wallace, 2021). While more resources have been developed to address this (Menage et al, 2021; Raynor et al, 2021), colonialism continues to manifest through the lack of diversity, especially in higher education in midwifery, and in global majority student experiences and outcomes (RCM, 2023b). The toolkit has four sections supported by evidence to assist in anti-racist practices: student recruitment, the curriculum, assessment and practice.
Midwifery students and staff additionally need to understand social inequalities, White privilege, and racism in all its forms, so that they can challenge this, speak up when it is witnessed (become an active bystander) and speak out against racism (Jieman et al, 2022; Playfair et al, 2023). Midwifery academics need to lead on these conversations in university and with practice partners. Examples of microaggressions can be discussed in class, such as asking someone ‘where they are from?’ and not trying to pronounce names properly. The Birthrights (2022) report, ‘systemic racism, not broken bodies’, acknowledged that healthcare professionals can fail to recognise that they are using stereotypes or microaggressions. Therefore, one of the first steps in tackling racism is understanding how personal actions affect others. Robust recommendations have been developed in relation to nursing education (Playfair et al, 2023); some of which are summarised in Table 1, alongside the Birthrights (2022) findings and further resources.
Table 1. Recommendations for nursing education
| Birthrights (2022) call to action | Playfair et al (2023) recommendations for educators | Further resources |
|---|---|---|
| Commit to being an anti-racist organisation | Institutional commitment to training and education to support and retain staff and students | Chartered Institute of Personnel and Development (2021) |
| Decolonise maternity curriculums and guidance | Teach about social determinants of health and how racism in society impacts health. Incorporate diverse teaching resources and methods | Royal College of Midwives (2023b) |
| Create safe, inclusive workforce cultures | Do not deny racism or say ‘I do not see colour’. Understand White privilege, even if it feels uncomfortable | Hemmings et al (2021) Hone (2020) |
| Dismantle structural barriers to racial equity through national policy change | Move from mandatory training on unconscious bias alone to anti-racist practices and allyship | Race Disparity Unit (2024) |
Conclusions
The UK position is not unique, despite higher education organisations globally committing to diversity and inclusion policies. The benefits of a diverse workforce in midwifery cannot be overstated, given the poor outcomes for women and their babies from global majority backgrounds, nationally and globally. The midwifery profession needs greater diversity in teaching staff, clinical midwives and midwifery students to reflect the diversity in the population and improve outcomes for global majority women, especially in maternity services.
Key points
- The lack of diversity in the midwifery profession is a major concern.
- Midwifery needs more students, registrants and academics from a global majority background.
- Global majority students, staff and academics face barriers that their White counterparts do not, including systemic racism.
- Action is required to make a positive impact for global majority midwifery students and staff but most of all for the women from global majority backgrounds who access maternity services.
CPD reflective questions
- Do you know what constitutes a microaggression? Do you hold colleagues to account if you hear these used in clinical practice, the classroom or workplace?
- Do you understand systemic racism and how representation and allyship can question and change entrenched practices for greater equality?
- Have you read the Royal College of Midwives decolonising midwifery educators toolkit?
- Have you watched the Nursing and Midwifery Council challenging discrimination videos? As a registrant, the Code states that everyone has the right to dignity and respect. The animation supports professionals to feel confident about challenging discriminatory behaviour.
- If you are White, have you reflected on your privilege?


