The rapid advancement of digital technologies has changed educational methodologies in var ious sectors, including healthcare education (Booth et al, 2021; Alammary et al, 2023; Wang et al, 2023; Aasekjær et al, 2024; Proença et al, 2024). With its immersive and interactive capabilities, virtual reality stands at the forefront of this educational revolution. Midwifery demands a high level of procedural knowledge and practical expertise, meaning that conventional pedagogical approaches may fall short (Abraha et al, 2023; Chaika, 2024). Conventional methods are typically centred around didactic instruction and limited patient interaction, which may not fully prepare students for the dynamic and complex realities of clinical environments (Gray et al, 2022; Abraha et al, 2023; Chaika, 2024).
Virtual reality simulates real-world scenarios, allowing midwifery students the opportunity to hone their skills without the inherent risks of live clinical settings. The benefits of virtual reality are well-documented across various educational fields, and include enhanced engagement and accelerated learning curves because of its immersive nature (Liu et al, 2023; O'Connor and Rainford, 2023; Fujiwara et al, 2024). However, the application of virtual reality in midwifery education has not been thoroughly explored. The existing literature, while optimistic about virtual reality's potential, often relies on fragmented studies or anecdotal evidence that lack comprehensive methodological rigor (Abraha et al, 2023; Alammary et al, 2023; Aasekjær et al, 2024; Chaika, 2024). This highlights the pressing need for systematic, empirical evaluations of virtual reality's impact on both the acquisition of clinical skills and broader educational outcomes in midwifery (Fealy et al, 2019; Gray et al, 2022).
This study aimed to assess the effectiveness of Virtual Medical Coaching's BirthWise virtual reality, compared to conventional simulation education methods using Lucy maternal and neonatal birthing simulators, in midwifery education. The study provides a holistic evaluation of virtual reality's educational value, contributing valuable insights to the ongoing discourse on innovative educational practices in healthcare. The findings are intended to inform future curriculum developments and support the integration of cutting-edge technologies in midwifery education, potentially reshaping educational standards and practices in the field (Slavin, 2002; Changuiti et al, 2023).
Methods
This prospective cohort study evaluated the impact of virtual reality technology (using BirthWise VR by Virtual Medical Coaching software) on midwifery education in comparison to conventional task trainers (Lucy maternal and neonatal birthing simulators). The study assessed these methodologies in relation to students' knowledge retention, skill acquisition and satisfaction. A mixed-methods approach was used that integrated quantitative and qualitative techniques to provide a comprehensive view of educational outcomes. This article reports the results of the quantitative branch of the study, with the qualitative results intended for a future publication.
Participants
The study involved all first-year midwifery students from two consecutive academic years at Kaaf University. Each cohort was exposed to one of two distinct education methods: the virtual reality cohort (n=46 students) were trained using immersive virtual reality simulations, while the conventional cohort (n=42 students) were trained using conventional task trainers.
The conventional cohort consisted of the entire class that preceded the acquisition of virtual reality technology at the university. This cohort had no access to virtual reality during their first year, as the technology was not yet available. However, they did use virtual reality in their second and third years of the degree. The data for this cohort were collected during their first year, before the introduction of virtual reality, ensuring that the subsequent virtual reality experience did not influence the results.
The intervention
The virtual reality simulations used Virtual Medical Coaching's BirthWise virtual reality, and provided comprehensive end-to-end sessions where students engaged in the complete birth process, from early labour through to skin-to-skin care, breastfeeding, placenta inspection and completing medical notes. This immersive environment replicated a fully functioning birthing suite, adaptable to various settings with minimal setup, allowing students to practice in diverse scenarios. The virtual reality simulations featured dynamic elements, such as maternal vital signs and fetal heart rate patterns, creating a realistic and interactive learning experience. Students were able to perform essential clinical tasks, including vaginal and cervical examinations to assess labour progress and make clinical decisions. Additionally, students palpated the fetus to assess its position and engagement, applying theoretical knowledge to realistic situations. The immersive nature of the virtual reality suite allowed students to practice decision making and problem solving in real-time, with immediate feedback on their actions.
The conventional simulation education used realistic manikins (Lucy maternal and neonatal birthing simulators) in high-fidelity simulation rooms designed to mimic a hospital-based birthing environment. The setup included a fully equipped birthing suite with all standard medical and midwifery equipment and environmental factors found in a hospital. The manikin-based education focused on manual skills and procedure familiarity, with students practicing techniques such as cervical examinations, manual birth, episiotomies and neonatal resuscitation. Each stage of childbirth was simulated separately, allowing students to concentrate on specific procedures and protocols. The simulation ward also featured two-way mirrors, enabling students to be observed and critiqued by both peers and instructors, enhancing the fidelity and authenticity of the experience.
Both groups were provided with task trainers for managing complications such as shoulder dystocia, breech birth and umbilical cord prolapse, encouraging the development of dexterity and muscle memory, and preparing students for emergency situations. Aside from the simulation style and equipment used, all lessons and instruction were the same between the cohorts, ensuring a consistent educational foundation across both groups.
Data collection
Students in both groups completed pre- and post-tests at the beginning (September 2021/2022) and end (June 2022/2023) of the academic year to quantitatively evaluate their theoretical knowledge and practical skills. The tests were administered in English at the university's simulation laboratory in the first and final weeks of the academic year for each cohort. Students were given 60 minutes to complete the test.
The learning outcomes assessed as part of the students' education programme focused on several critical competencies essential for professional practice. Students were evaluated on their clinical competence, particularly their ability to perform key midwifery skills, such as comprehensive maternal assessments, managing normal labour and birth and providing postpartum care. Another core area of assessment was evidence-based practice, where students demonstrated their ability to critically evaluate and apply the latest research to inform clinical decisions. The education programme also emphasised professionalism and ethics, assessing students' adherence to ethical standards and legal frameworks, as well as their cultural sensitivity and respect for patient autonomy. Finally, students' critical thinking and problem-solving abilities were rigorously assessed, particularly their capacity to analyse complex clinical situations, develop appropriate care plans and respond effectively to emergencies during childbirth. These outcomes ensure that graduates are well-prepared to meet the demands of midwifery practice.
The tests were developed by a multidiscplinary team of educators and clinical midwives from the university, aligning with the core competencies of the midwifery curiculum. Input was sought from experts in educational assessment to ensure relevance and rigour. The tests were piloted with a separate group of midwifery students from a previous cohort. Their feedback was used to refine question clarity and ensure that the tests effectively measured the intended competencies.
The test had 40 questions divided into three sections. The first section (10 multiple choice questions) focused on theoretical knowledge, covering core midwifery concepts. The second section (15 short-answer questions) required students to provide concise written responses on critical reasoning, such as explaining steps in a specific procedure or interpreting clinical data. The third section (15 scenario-based questions) evaluated practical decision making skills, where students outlined their approach to clinical cases, justified their decision and prioritised care steps.
Data analysis
The Mann-Whitney U test was used to compare pre- and post-test scores, with P<0.005 used to indicate significance. Age distribution was assessed using an independent t-test. Differences in satisfaction, effectiveness and confidence between cohorts were assessed using a t-test. Histograms with Kernel density estimate plots were created for participants' scores. Kernel density estimates are a non-parametric way to estimate the probability density function of a random variable, providing a smooth curve that represents the distribution of the data. This technique is particularly useful for visualising the distribution of scores, as it helps to identify patterns and differences that may not be evident from histograms alone (Rosenblatt, 1956).
Ethical considerations
Ethical approval for the study was obtained from the Ghana Health Service Ethics Review Committee (reference: 2021-UG-15988). Detailed study information was provided to all participants, and consent was obtained prior to their training, ensuring that they understood that their data would be collected and used for research purposes. Distinct consent forms were developed for each cohort, with the virtual reality cohort's form explaining the use of immersive virtual reality simulations and the conventional cohort's form clarifying the use of conventional task trainers. Participation was entirely voluntary, and had no impact on education or grades, and all data were anonymised to maintain confidentiality.
Results
Table 1 shows a comparison between virtual reality and traditional cohorts across various metrics. Initial assessment indicated no significant difference in pre-test scores between the virtual reality and traditional cohorts, confirming a comparable baseline (P=0.657). However, significant differences emerged in both the post-test and practical test scores, where the virtual reality cohort markedly outperformed the traditional group (post-test scores: P<0.0001; practical test scores: P<0.0001). To ensure that age did not confound the results, an independent t-test was performed, showing no statistically significant difference between the cohorts' age groups (t=- 0.5, P=0.62), verifying that the age distribution was effectively controlled.
| Metric | Group | Mean scores/age | Test statistic | P value | Notes |
|---|---|---|---|---|---|
| Pre-test score comparison | Virtual reality | 56.20 | Mann-Whitney U=1000.0 | 0.043 | Virtual reality outperformed slightly |
| Traditional | 54.90 | ||||
| Post-test score comparison | Virtual reality | 78.40 | Mann-Whitney U=1200.0 | <0.0001 | Virtual reality outperformed significantly |
| Traditional | 73.10 | ||||
| Practical test score comparison | Virtual reality | 92.00 | Mann-Whitney U=1300.0 | <0.0001 | Virtual reality outperformed significantly |
| Traditional | 87.00 | ||||
| Age distribution | Virtual reality | 31.50 | t=-0.5 | 0.62 | Not statistically significant |
| Traditional | 32.00 | ||||
| Satisfaction | Virtual reality | 85.00 | t(85)=11.00 | <0.0001 | High in virtual reality |
| Traditional | 75.00 | ||||
| Perceived effectiveness | Virtual reality | 95.00 | t(85)=10.50 | <0.0001 | Virtual reality perceived as highly effective |
| Traditional | 84.00 | ||||
| Confidence in clinical application | Virtual reality | 90.00 | t(85)=9.50 | <0.0001 | Higher confidence with virtual reality training |
| Traditional | 80.00 |
In statistical analysis, the virtual reality cohort rated their education as significantly more effective (P<0.0001), expressed greater satisfaction (P<0.0001) and showed higher confidence in their clinical skills (P<0.0001) compared to the traditional cohort.
Figure 1 shows histograms with overlaid Kernel density estimate plots for both education methods. The plots highlight the superior performance of the virtual reality cohort, showing a higher concentration of scores in the upper range, indicating that students trained with virtual reality achieved better overall outcomes compared to those trained with traditional methods. Figure 2 shows the progression of scores from pre-to post-test for both cohorts, clearly showing the virtual reality cohort's higher trajectory and overall better performance in post-test evaluations.
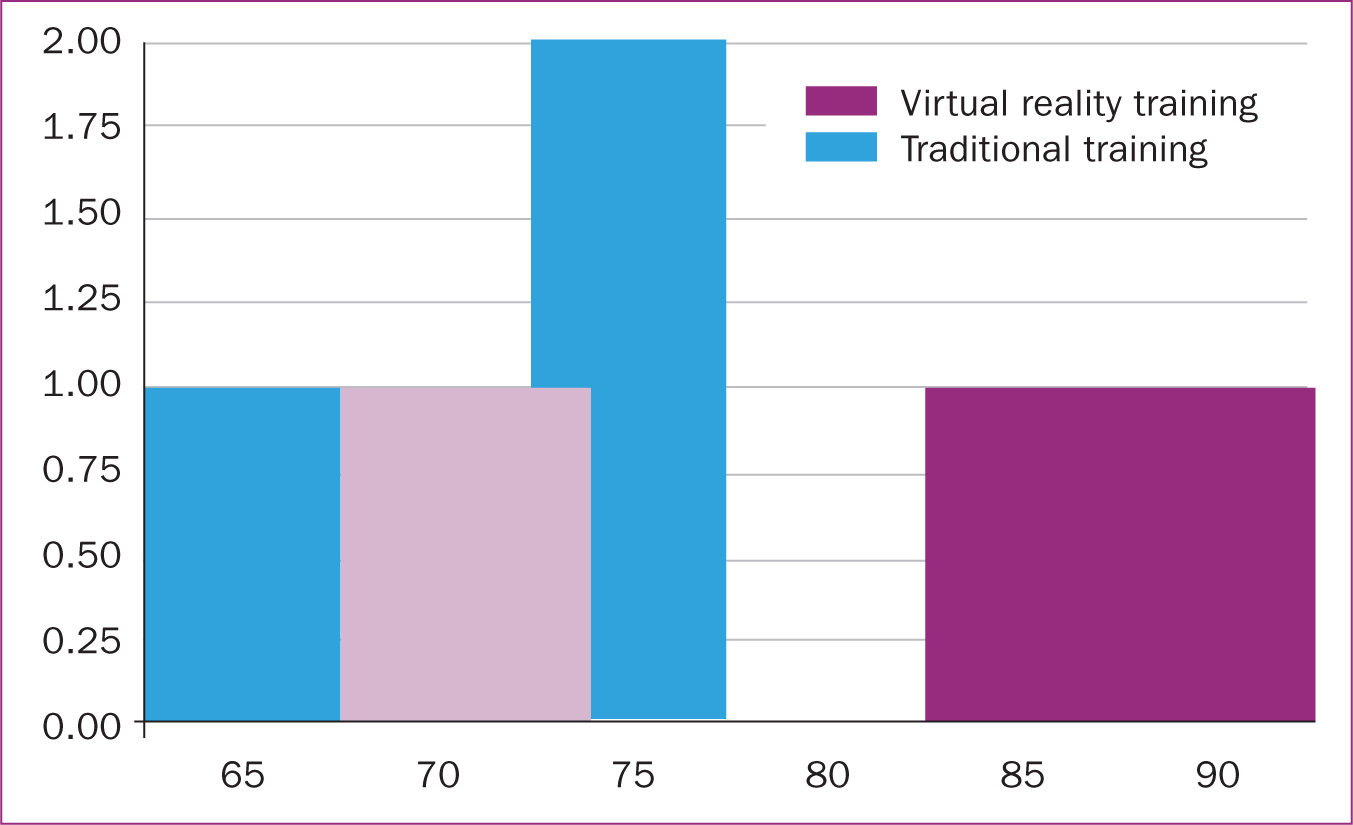
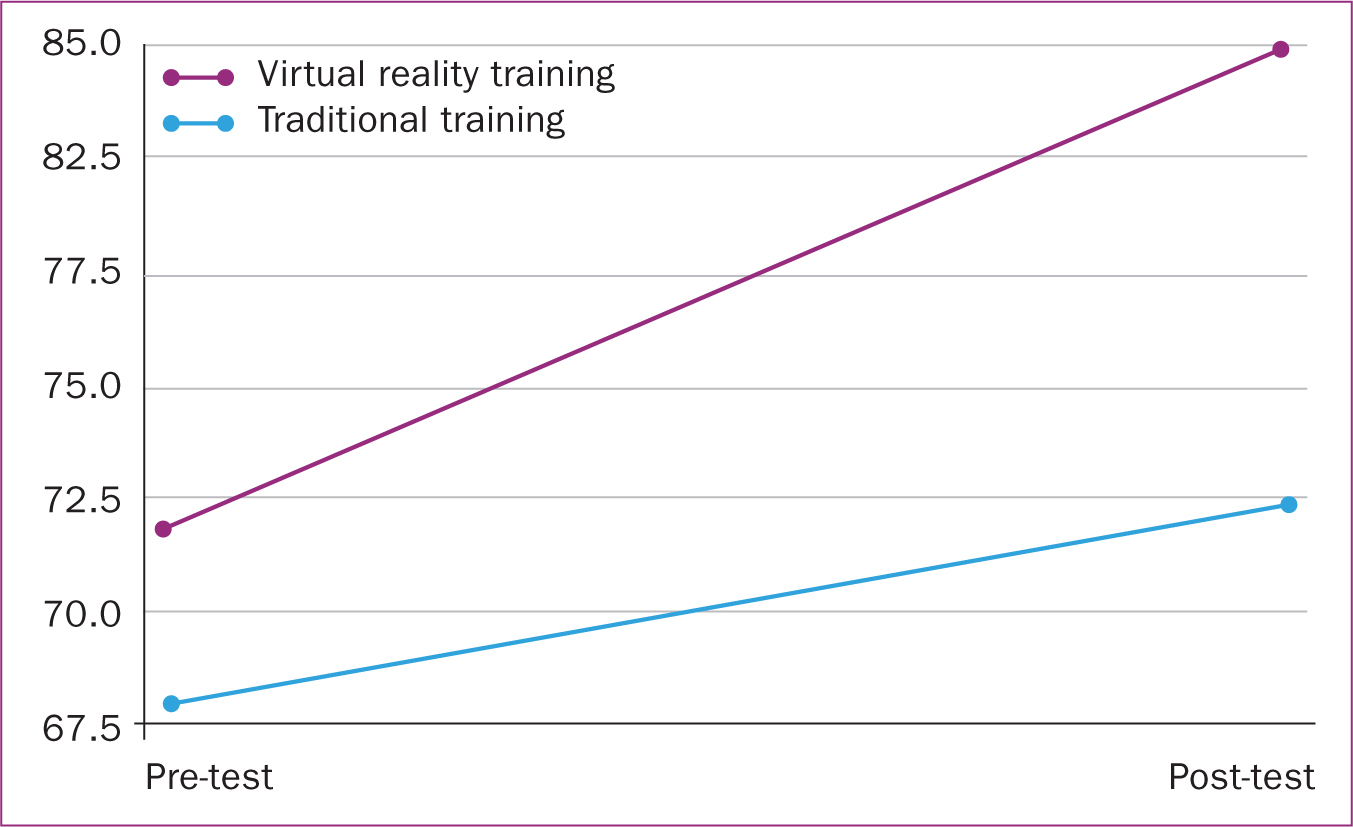
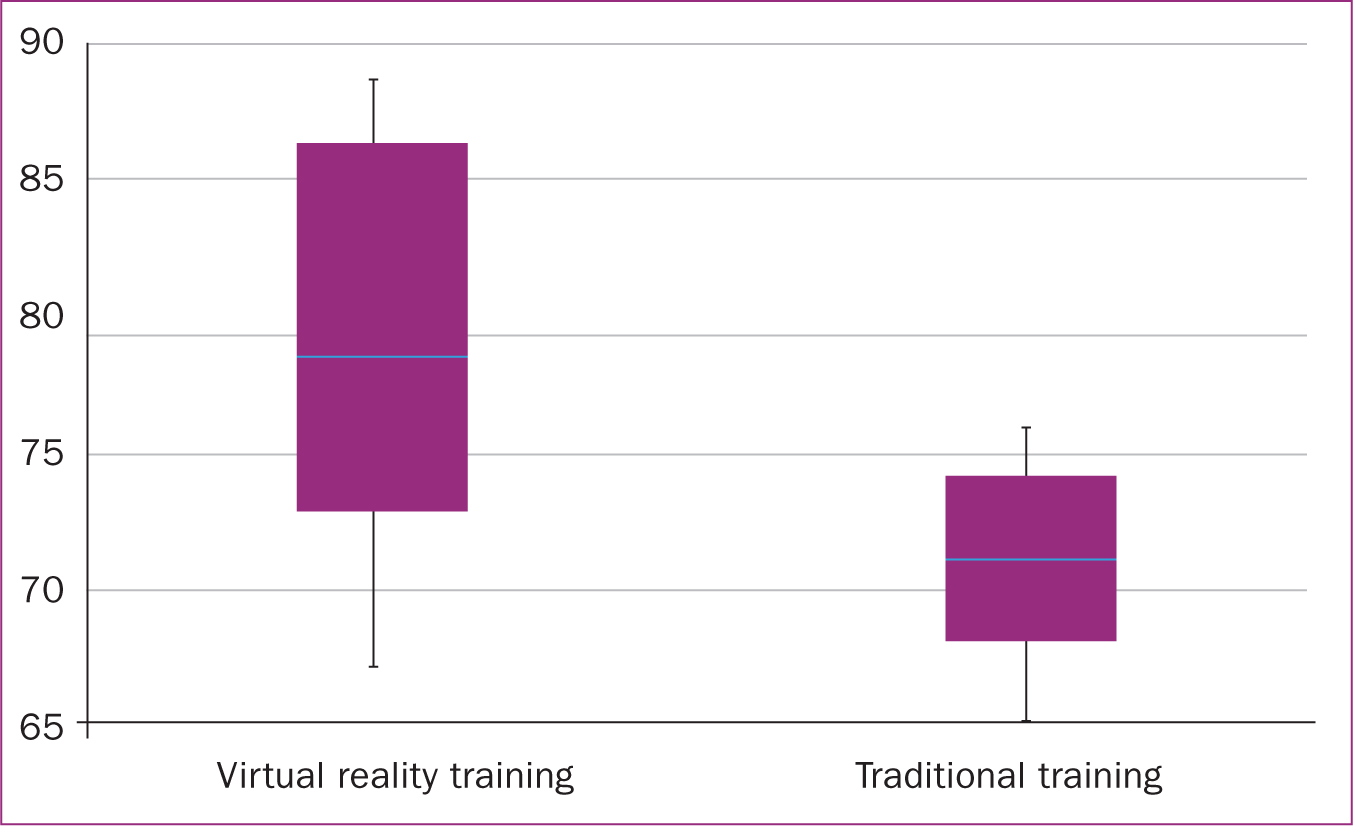
Figure 3 shows box plots that contrast the score distributions between the virtual reality and traditional education methods. These plots show median, quartiles and outliers, providing a detailed visual comparison of the data's spread and central tendencies in each group. The results demonstrate that virtual reality training significantly enhanced learning outcomes, increased student engagement and improved students' practical skills.
Discussion
This study's findings strongly emphasise the benefits of virtual reality simulation over conventional task trainers in midwifery education. The quantitative analyses highlighted that virtual reality's immersive and interactive nature significantly enhanced student preparation for professional midwifery roles, offering a more effective educational tool that better equipped students with essential skills and confidence. This conclusion is further supported by international research in other allied health professions. Virtual reality simulation has been shown to provide substantial benefits in nursing, physical therapy and medical training, consistently improving skill acquisition, confidence and clinical decision making compared to traditional training methods (Allcoat and von Mühlenen, 2018; Vesisenaho et al, 2019; Cook and Lischer-Katz, 2020; Meese et al, 2021; Woon et al, 2021).
The virtual reality simulations allowed students to engage in complete birth processes, from early labour through to postpartum care, including the inspection of the placenta and the completion of medical notes. This comprehensive and realistic approach enables students to gain a full understanding of the entire birthing process, not just isolated skills. Holistic training ensures that students are well-prepared for the full scope of midwifery practice, which is crucial for building confidence and competence in real-world clinical settings.
Replicating a fully functioning birthing suite in a virtual reality environment provided students with a training setting that closely mirrored what they will encounter in actual clinical practice. This realistic simulation reduces the gap between theoretical learning and real-world application, ensuring that students are better equipped to handle the complexities and unpredictability of labour and birth (Cook and Lischer-Katz, 2020). Incorporating dynamic elements, such as maternal vital signs and fetal heart rate patterns, significantly enhanced the realism of the virtual reality simulations. These features not only helped in the development of critical decision-making skills under pressure but also allowed students to practice responding to changing clinical scenarios in real-time, an essential aspect of effective midwifery practice.
The immediate feedback provided in the virtual reality environment allowed students to learn from their mistakes and adjust their approaches. This iterative learning process is crucial for refining skills and building the quick-thinking and adaptability required in high-stakes situations, such as childbirth (Kyaw et al, 2019; Pottle, 2019; Lange et al, 2020; Meese et al, 2021; Sung et al, 2024).
The study highlighted the limitations of conventional manikin-based education, such as a lack of engagement and realism. The need for more interactive and immersive training methods was apparent, and virtual reality offered more effective preparation for the students, addressing deficiencies found in traditional methods. The enhanced engagement and satisfaction reported by virtual reality-trained students suggest that virtual reality not only improved learning outcomes but also made the educational process more enjoyable and rewarding. This is particularly important in midwifery, where retaining skilled professionals is critical to addressing workforce shortages and ensuring high standards of care (Kyaw et al, 2019; Pottle, 2019; Liaw et al, 2020; Buchman et al, 2022; Sung et al, 2024).
The virtual reality cohort exhibited notable improvements in knowledge retention and practical skills, compared to the traditionally trained cohort, in both post-tests and practical assessments. This marked improvement can be attributed to the realistic, interactive and engaging educational experiences facilitated by virtual reality environments, echoing findings from prior research (Pottle, 2019; O'Connor and Rainford, 2023; Rainford et al, 2023; Aasekjær et al, 2024).
The participants praised the realism and complexity of clinical scenarios presented in virtual reality. Their increased preparedness and confidence were credited to the direct, hands-on practice and immediate feedback offered by virtual reality simulations. This feedback mechanism aligns with educational theories that champion experiential learning environments, which are proven to enhance cognitive assimilation and skill proficiency through active, realistic practice scenarios (Kyaw et al, 2019; Lange et al, 2020; Matthews, 2021; Meese et al, 2021; Jung, 2022; Alammary et al, 2023; Sung et al, 2024).
Conversely, the students criticised traditional education methods for their lack of engagement and realism, which mirrors previous work by Kavanagh et al (2017). Students expressed concerns about being underprepared for the unpredictability of real-life clinical settings. This underscores a significant deficiency in traditional midwifery education, suggesting a pivotal area for improvement by integrating more interactive and realistic education elements.
Future studies should track virtual reality-trained students in their professional practice to assess the long-term impact on clinical performance and patient outcomes. Conducting randomised controlled trials will help mitigate potential cohort effects and provide stronger causal evidence of the benefits of virtual reality education. Further exploration into the cost-effectiveness of virtual reality implementations and its applicability across different healthcare disciplines will help verify its versatility and effectiveness. By addressing these areas, future research can refine virtual reality educational strategies to meet the evolving demands of healthcare education and ultimately improve patient care outcomes.
Implications for practice
The significant improvements in knowledge retention and practical skills among virtual reality-trained students provide strong evidence that virtual reality is a more effective training tool than conventional methods. These findings have important implications for curriculum development, suggesting that virtual reality should be a key component of midwifery education to ensure that graduates are well-prepared for clinical practice. Continuous evaluation and refinement of virtual reality educational strategies are crucial to ensuring that midwifery education keeps pace with technological advancements and meets the evolving needs of healthcare.
Limitations
The non-randomised design and reliance on cohorts from consecutive academic years might have introduced cohort effects that could skew the outcomes. Additionally, while the study focused on immediate learning outcomes, it did not explore the long-term retention of knowledge and skills or impact on clinical performance (Shalem and De Clercq, 2022).
Implementing randomised controlled trials in educational environments, especially in specialised fields like midwifery, presents significant challenges. These include logistical hurdles in standardising conditions, ethical concerns over equity and informed consent, and methodological difficulties in blinding and outcome measurement. Addressing these challenges requires innovative trial designs and robust collaborative frameworks to ensure randomised controlled trials are ethical and yield valid results.
Conclusions
This study found that virtual reality education markedly enhanced midwifery education. The immersive nature of virtual reality not only bolstered learning outcomes but also better equipped students for the rigorous demands of clinical practice. Given these substantial benefits, it is imperative for educational policymakers and academic institutions to consider the integration of virtual reality technologies into their curricula to more effectively prepare future healthcare professionals.


